
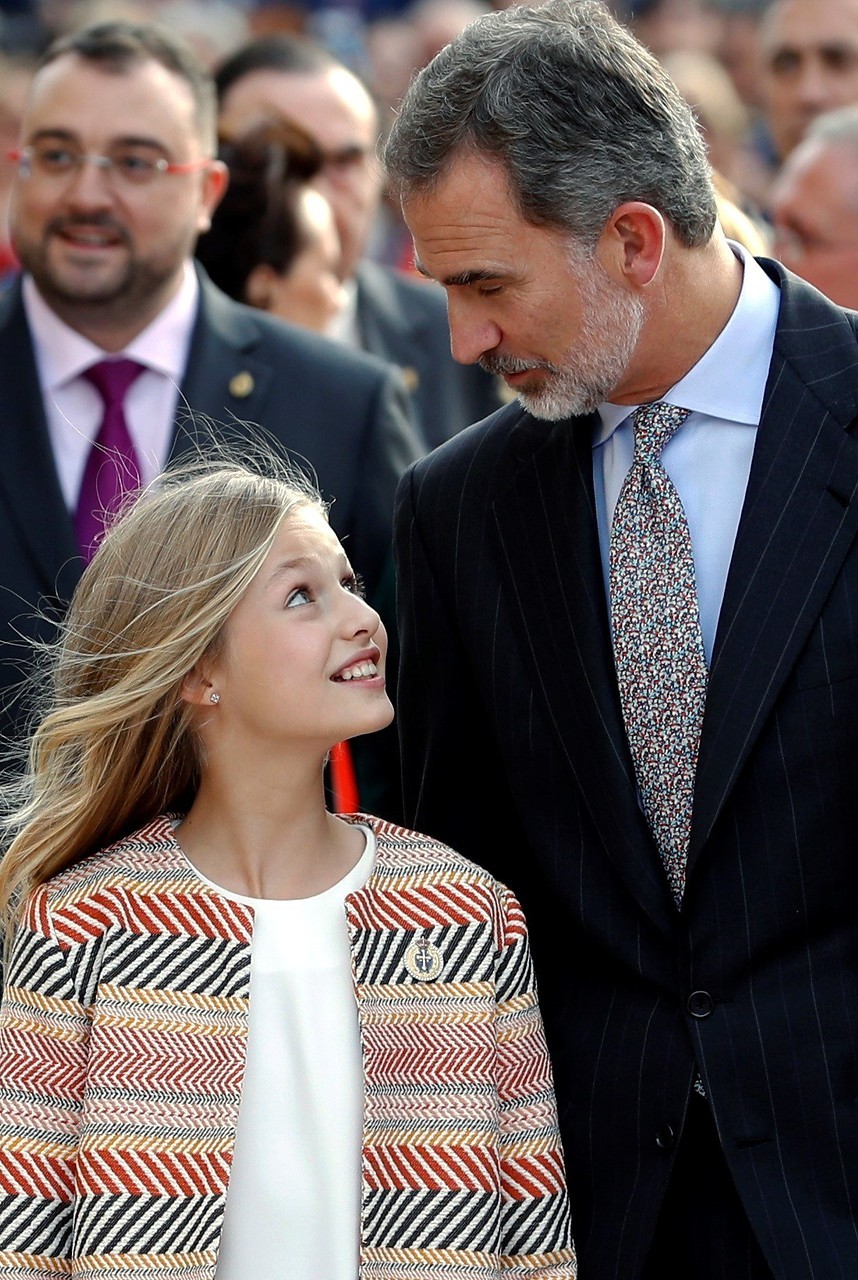
Las mochilas de Leonor y Sofía van con mensaje: sus adornos y llaveros, un guiño a sus aficiones | Vanity Fair

Son la princesa Leonor y la infanta Sofía las únicas princesas que no posan en la puerta del colegio? | La infanta, Infanta sofia, Tercer embarazo

La princesa Leonor y la infanta Sofía acuden a clase a pesar del caso coronavirus confirmado en su colegio

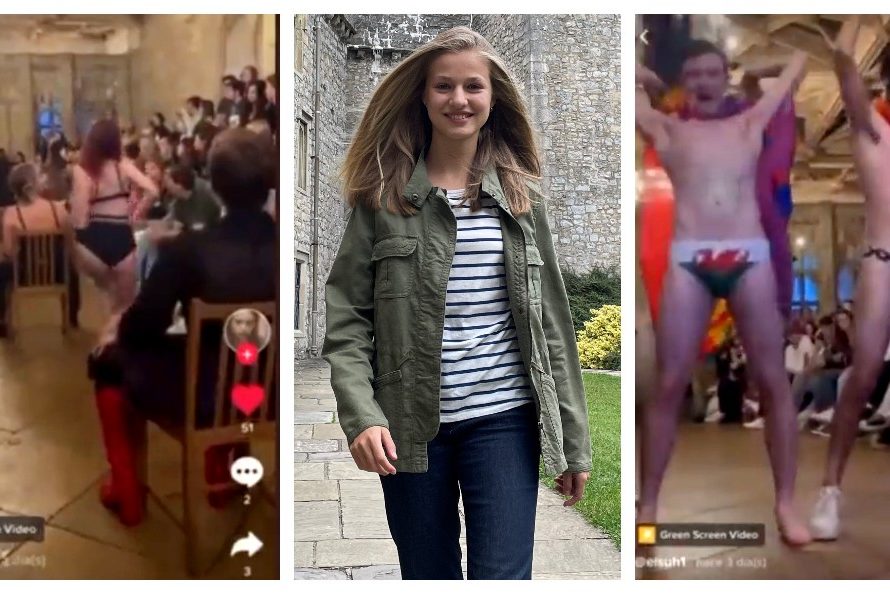
Por qué la realeza europea envía a sus hijos al 'Hogwarts Hippie': la influencia de los Windsor más allá de su país | Vanity Fair

internado DE PRINCESAS: La conexión secreta de la reina Sofía con el colegio de Gales de sus nietas | Mujer Hoy

Así es el exclusivo internado en Gales donde estudiará bachillerato la Princesa Leonor de Borbón (Felipe VI y la Reina Letizia van a pagar de su bolsillo los 75.000 euros al año








:format(jpg)/f.elconfidencial.com%2Foriginal%2Fe40%2F6ed%2F7dd%2Fe406ed7dd655ea13a1556dfa4122e8d2.jpg)





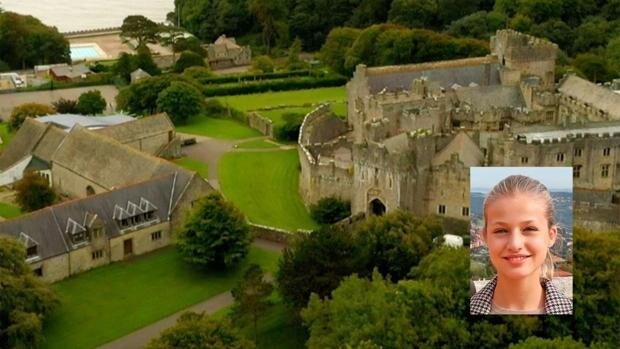
:format(jpg)/f.elconfidencial.com%2Foriginal%2Fba0%2F9d5%2Fcde%2Fba09d5cde0bdef63057d91c1fdd9f03b.jpg)
