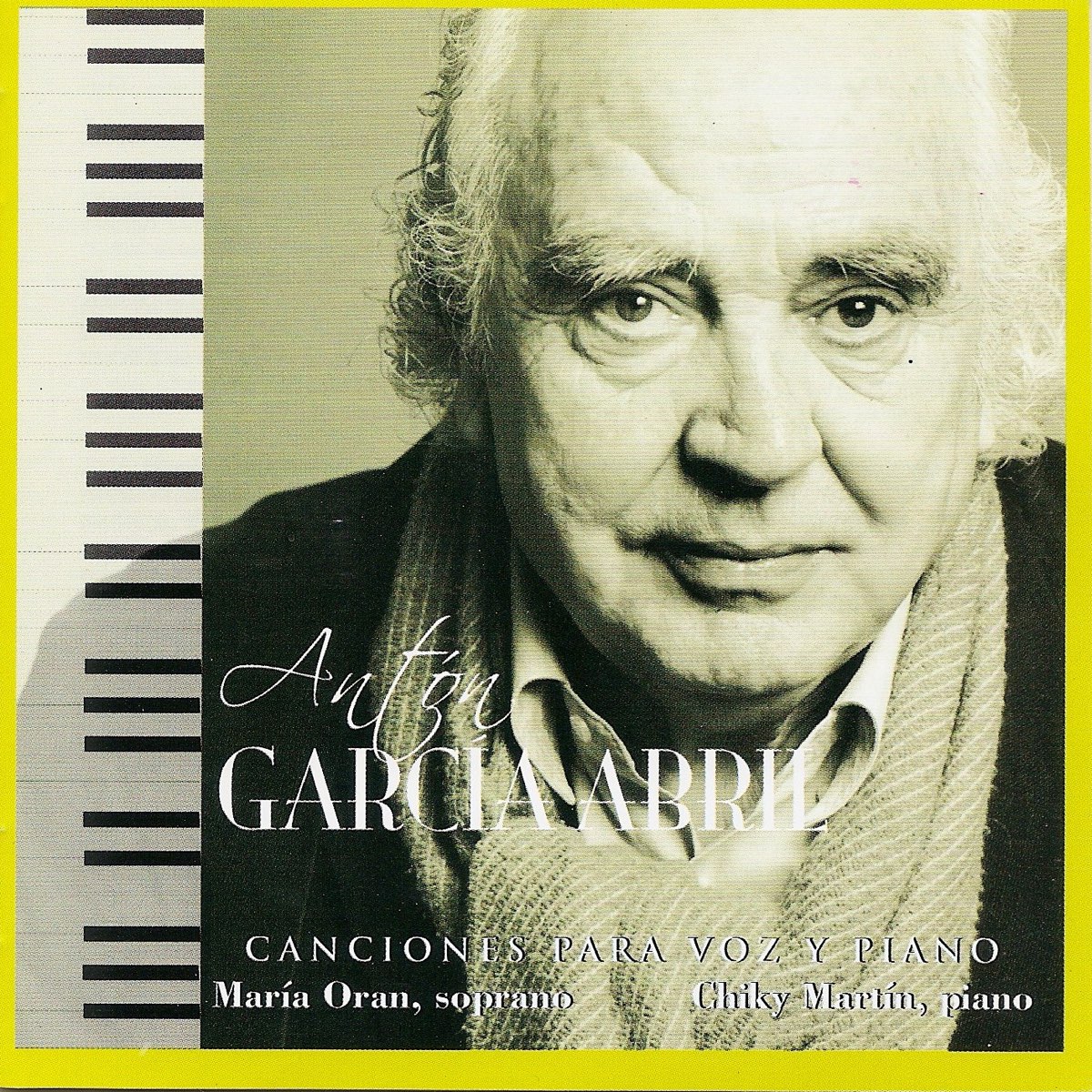
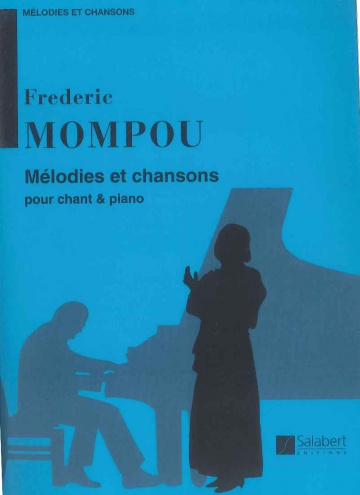
Partituras y ediciones críticas · Canciones de España, vol. 2, para voz y piano · VV. AA.: Unión Musical Ediciones S. L. -978-0-7119-6985-8 · El Argonauta. La librería de la música.
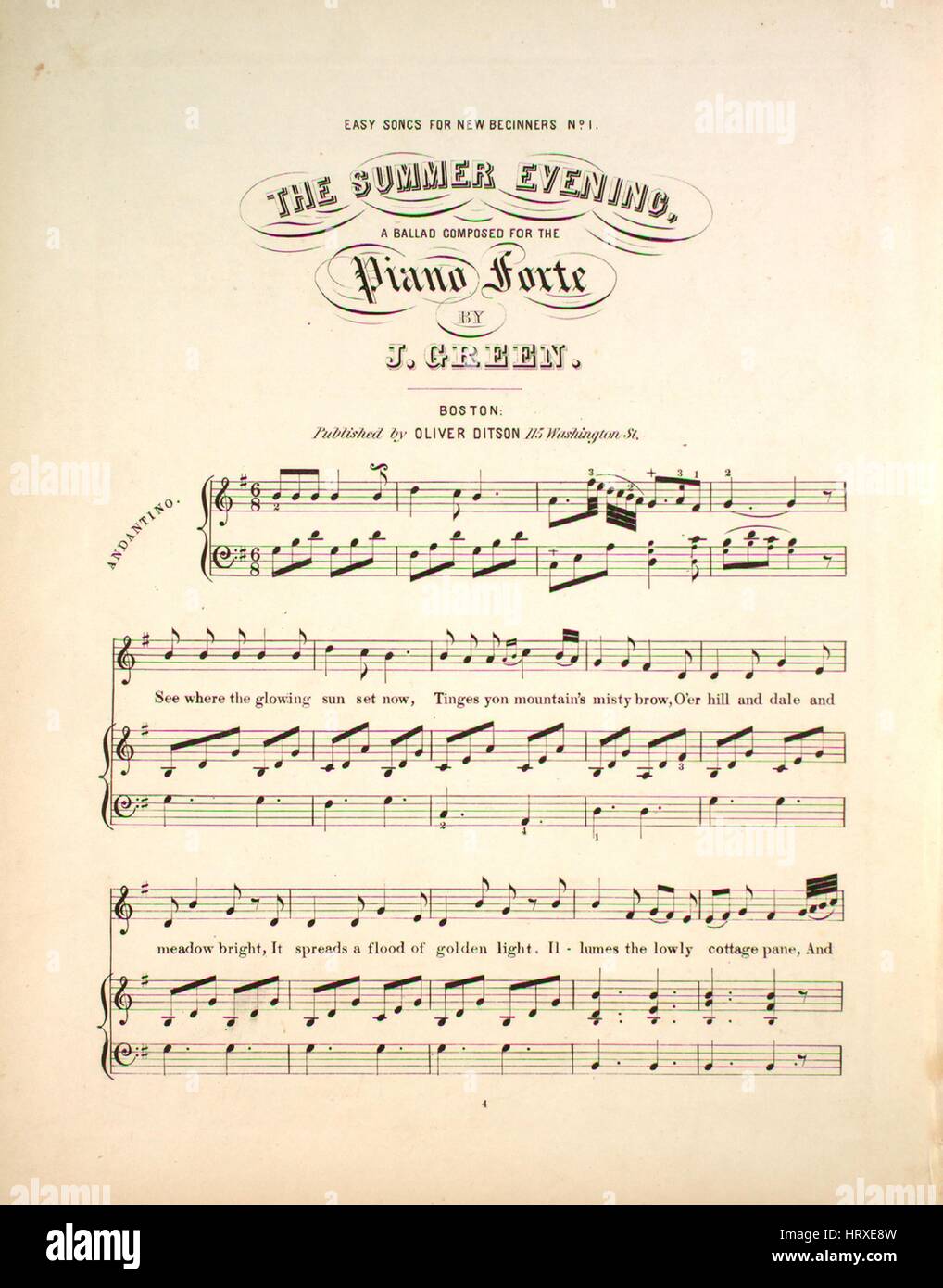
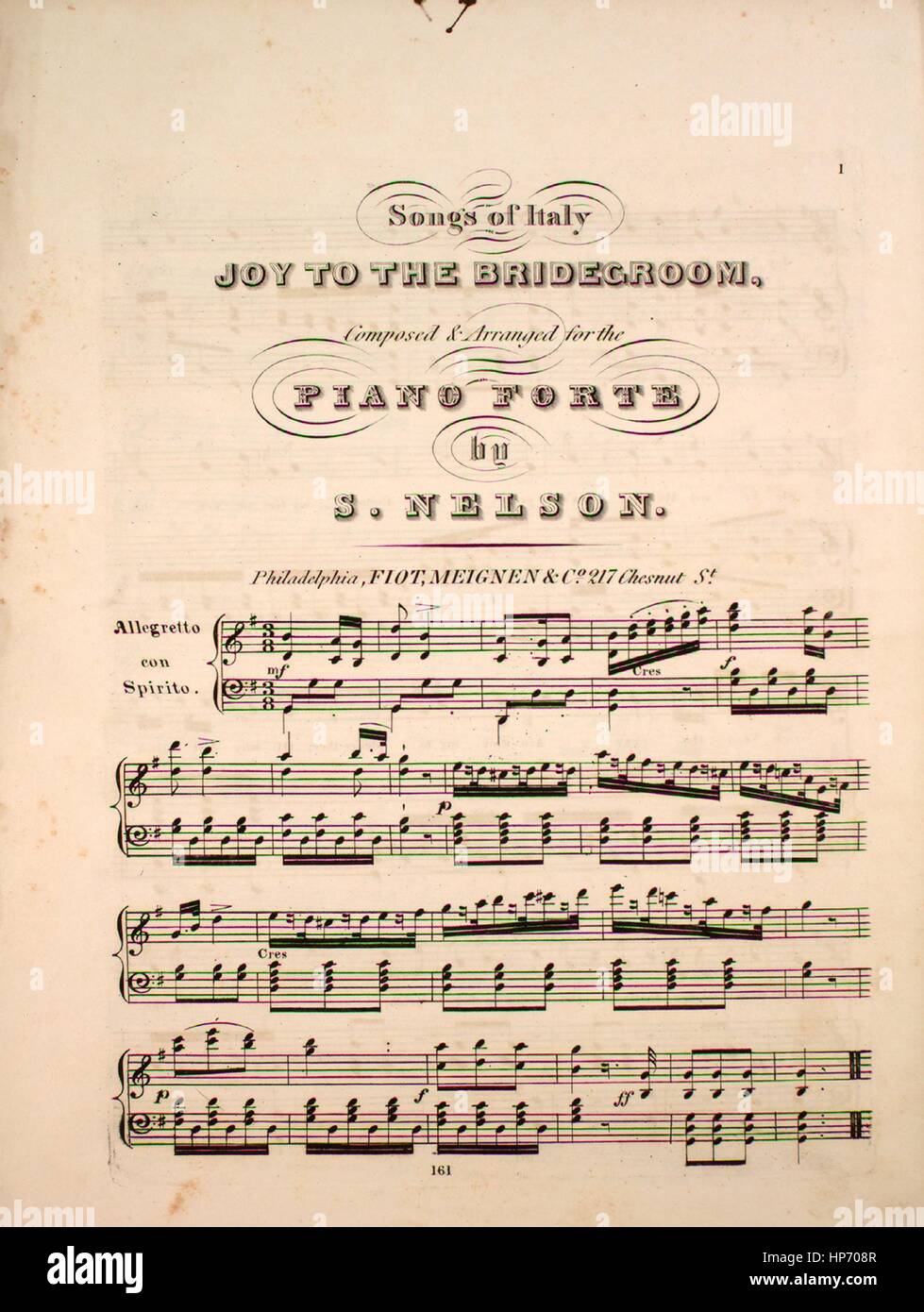
Imagen de cubierta de partituras de la canción 'Easy Canciones para los principiantes no 1 la noche de verano", con notas de autoría original leyendo 'Una balada compuesta para piano Forte por

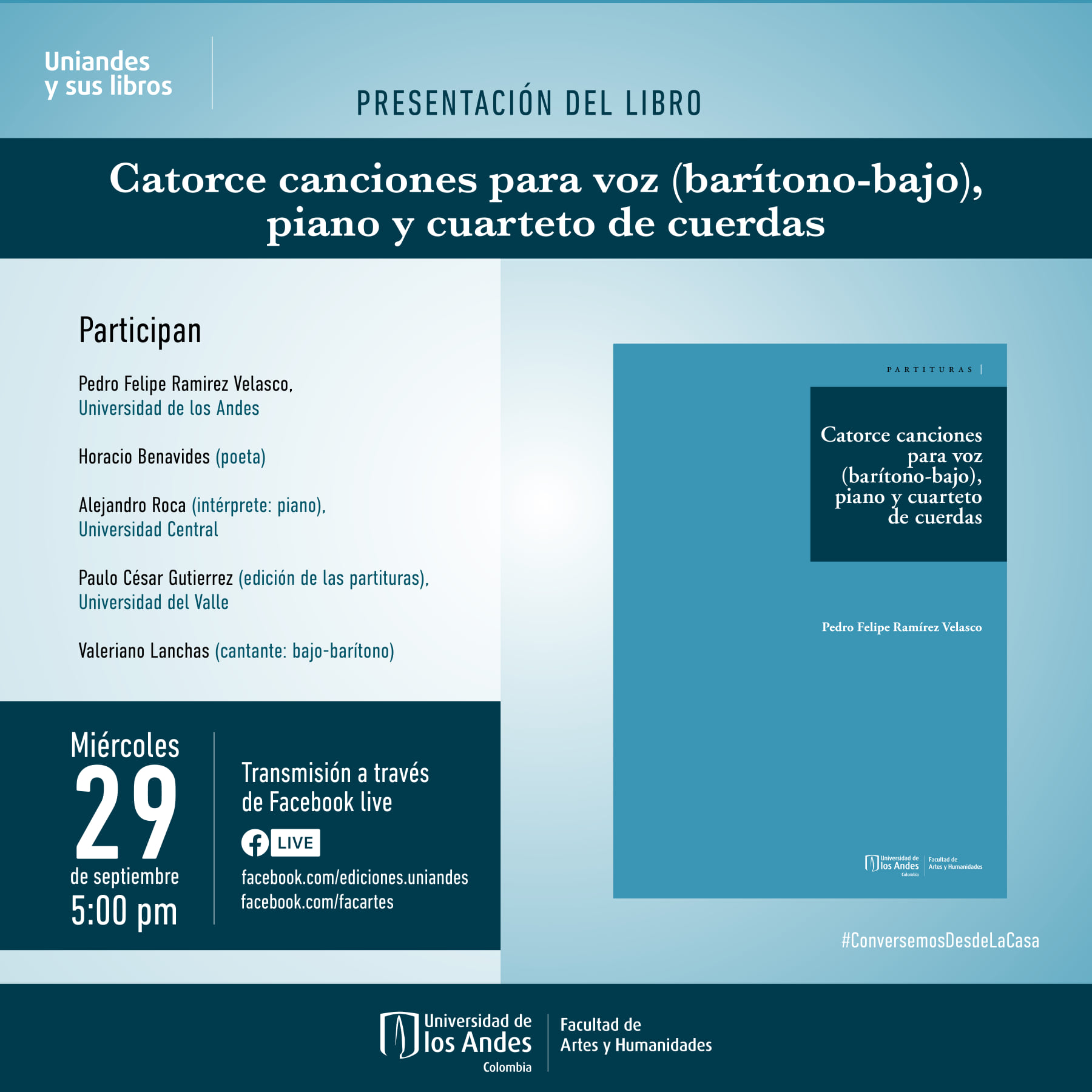
Amazon.com: Tres ciclos de canciones para VOZ y piano voz baja (Contralto o Bajo): 9786074507317: unknown author: Books