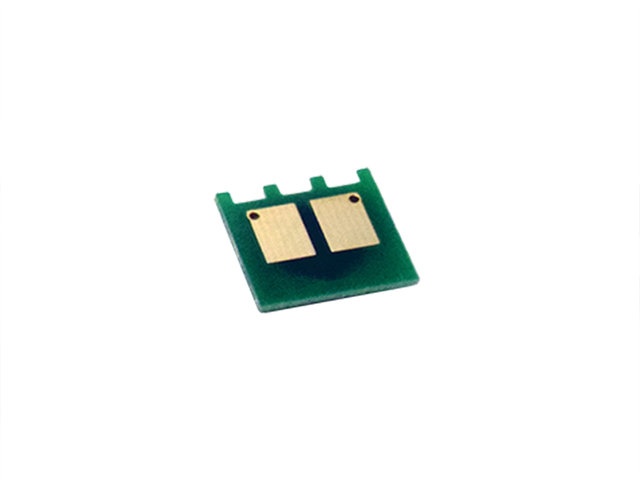
Toner Bank 2-Pack Compatible Toner Cartridge for HP CF279A 79A LaserJet Pro M12w M12a LaserJet Pro MFP M26nw M26a (Black) - Walmart.com

Amazon.com: HP 79A Black Toner Cartridge | Works with HP LaserJet Pro M12 Series, HP LaserJet Pro MFP M26 Series | CF279A : Office Products

Amazon.com: DIGITONER Compatible with HP 79 HP 79A HP CF279A Toner Cartridge HP– CF279A High Yield Toner Cartridge Replacement for HP Laser Printer Laserjet Pro M12w M12a MFP M26a M26nw – Black [

79A Compatible 79A Toner Cartridge 79A | CF279A Replacement for HP CF279A Pro M12w M12a MFP M26a M26nw Printer (Black, 2 Pack) - Walmart.com

HP 79A Black Toner Cartridge | Works with HP LaserJet Pro M12 Series, HP LaserJet Pro MFP M26 Series | CF279A : Office Products - Amazon.com