
Burger King España - Llegan al #KingJRMeal las Barbies, junto a Hot Wheels, con todo su flow. ¡Colecciónalos! | Facebook
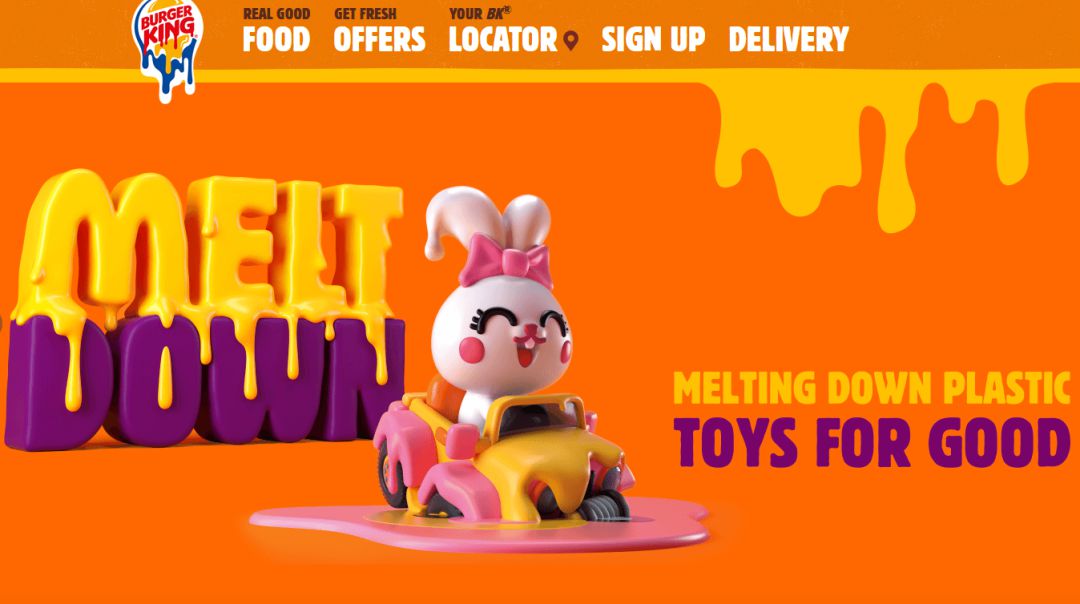
Burger King y McDonald's dejarán de regalar juguetes de plástico con sus menús infantiles | Ocio y cultura | Cadena SER


















:format(jpg)/f.elconfidencial.com%2Foriginal%2F6e2%2F2fa%2F2e3%2F6e22fa2e381f14de623c341d1d57ccee.jpg)

