Amazon.com: MTV Ao Vivo: Ivete Sangalo : Gilberto Gil, Margareth Menezes, Tatau, Daniela Mercury, Davi Moraes, Sandy, Sandy & Junior: CDs & Vinyl

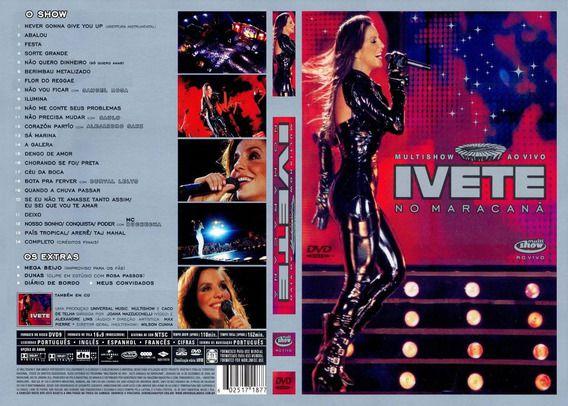
Amazon.com: Ivete - Multishow ao Vivo no Maracana : Ivete Sangalo, Samuel Rosa, Saulo, Alejandro Sanz, Durval Lelys, Buchecha: Movies & TV





![Thiago Aquino, Ivete Sangalo - Minha Condição [DVD Arrocha, Meu Lugar É Aqui] - YouTube Thiago Aquino, Ivete Sangalo - Minha Condição [DVD Arrocha, Meu Lugar É Aqui] - YouTube](https://i.ytimg.com/vi/OE615cNyHt8/maxresdefault.jpg)

/i.s3.glbimg.com/v1/AUTH_59edd422c0c84a879bd37670ae4f538a/internal_photos/bs/2018/U/s/0q5SY5R9umwLGAauDklg/ivete-sangalo-rafa-mattei.jpg)