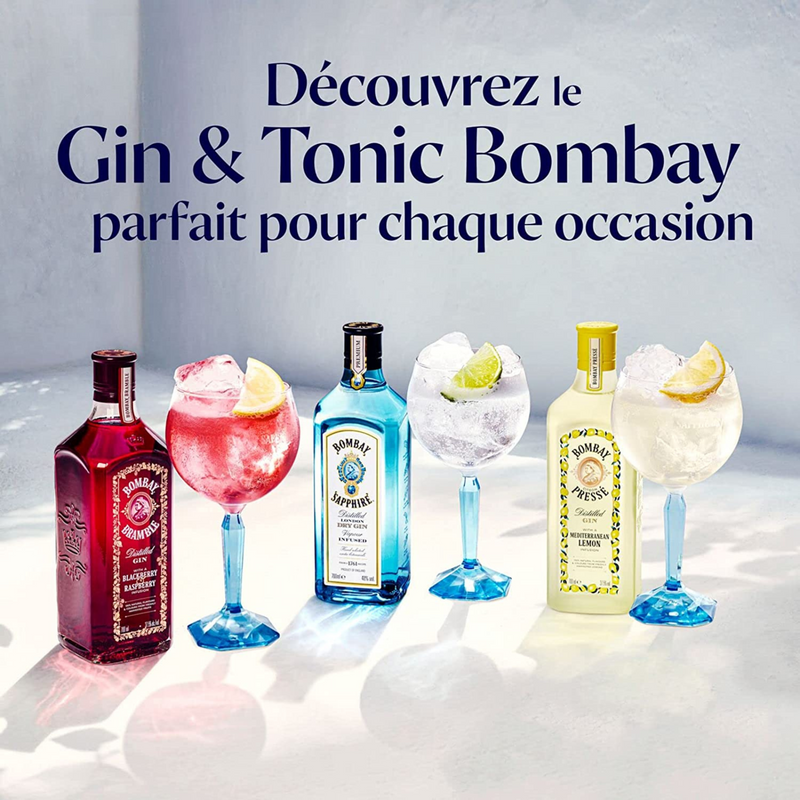
Un Gin Tonic Fraîchement Préparé Avec Des Tranches De Citron Et Une Cuillère Sur La Table | Photo Premium

Doodle Cartoon Gin Tonic Cocktail Et Composition Des Ingrédients Une Bouteille De Gin Et Deau Tonique Une Boule De Citron Et De Glace Pour Le Menu Du Bar Les Autocollants Ou La

Closeup Of Barman Hand Pouring Drink With Special Spoon On A Glass To Prepare Gin Tonic Cocktail Stock Photo, Picture and Royalty Free Image. Image 28422183.

Citrus Gin Tonic Lemon Orange Lime Zest Spiral Spoon Cardamom Stock Photo by ©VictorSantacruz 429194856

Gin Tonic With Lemon And Botanics In A Balloon Glass On Grey Background. With Bar Spoon And Measure Cup. Stock Photo, Picture and Royalty Free Image. Image 38742555.

Matériel Pour Préparer Gin Tonic Avec Des Botanicals Et La Cuillère De Barre Sur La Table En Bois Image stock - Image du ballon, mesure: 70691477

Matériel Pour Préparer Gin Tonic Avec Des Botanicals Et La Cuillère De Barre Sur La Table En Bois Image stock - Image du ballon, mesure: 70691477

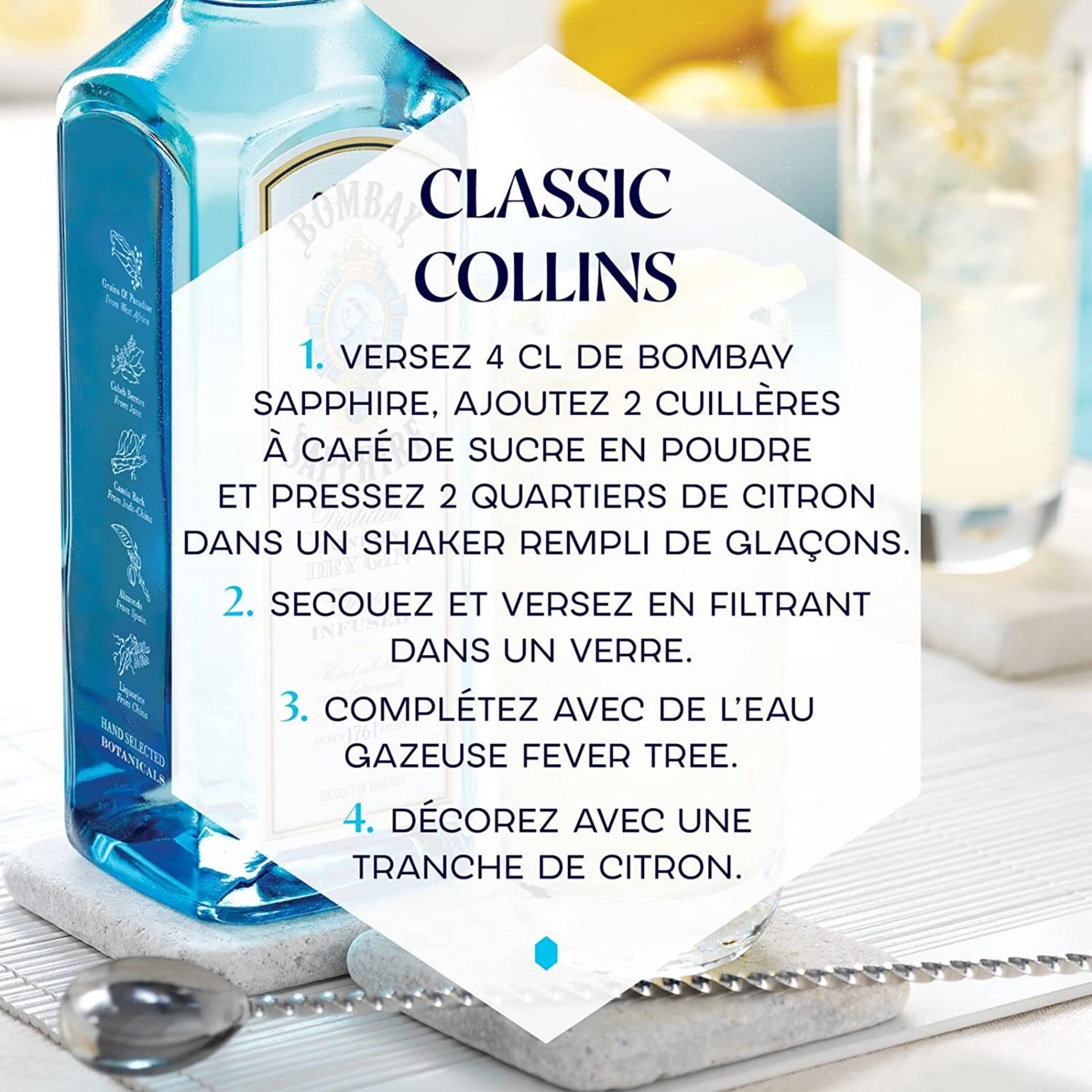
Un Gin Tonic Fraîchement Préparé Avec Des Tranches De Citron Et Une Cuillère Sur La Table | Photo Premium