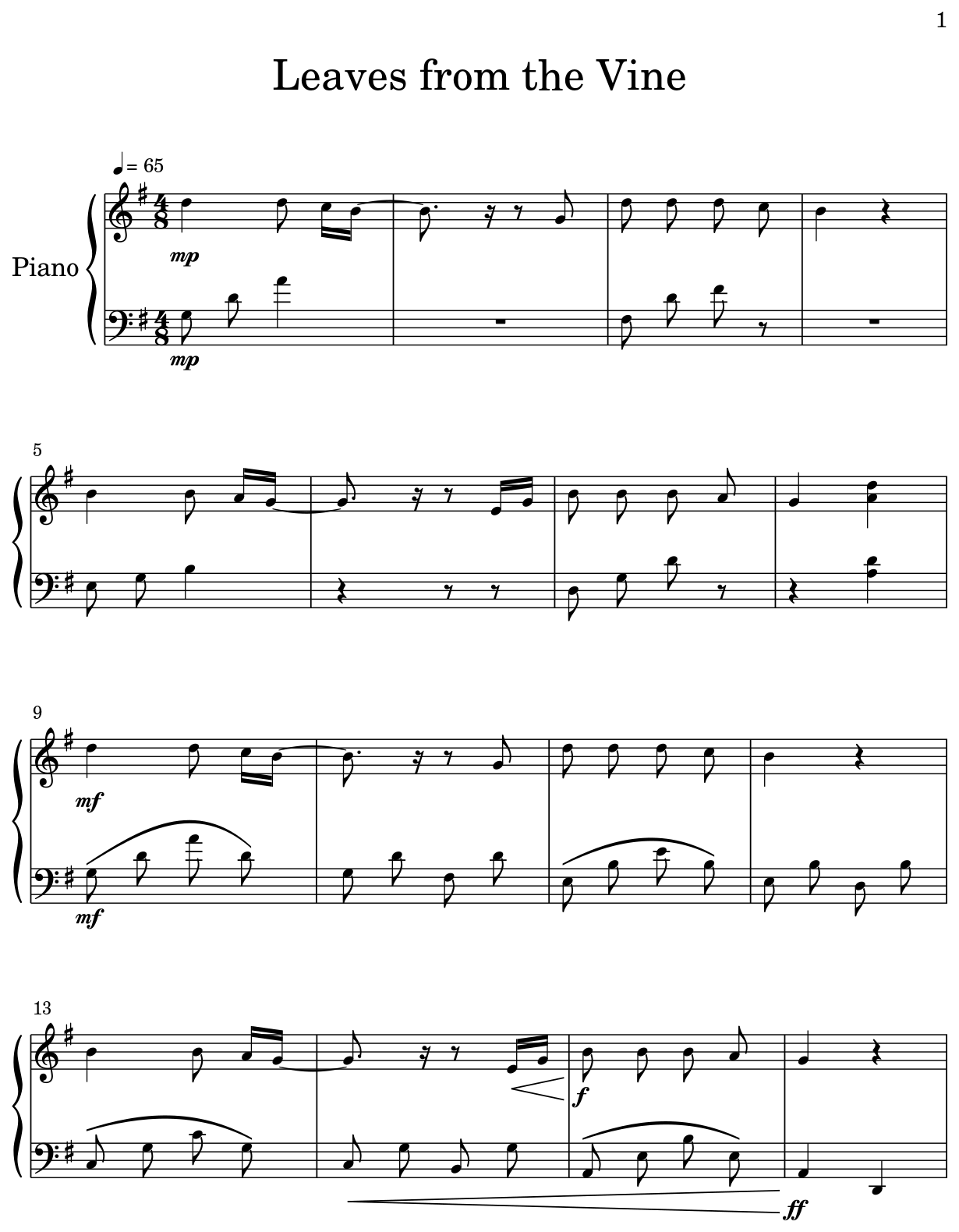
AtinPiano "Leaves from the Vine" Sheet Music (Piano Solo) in A Major - Download & Print - SKU: MN0214626

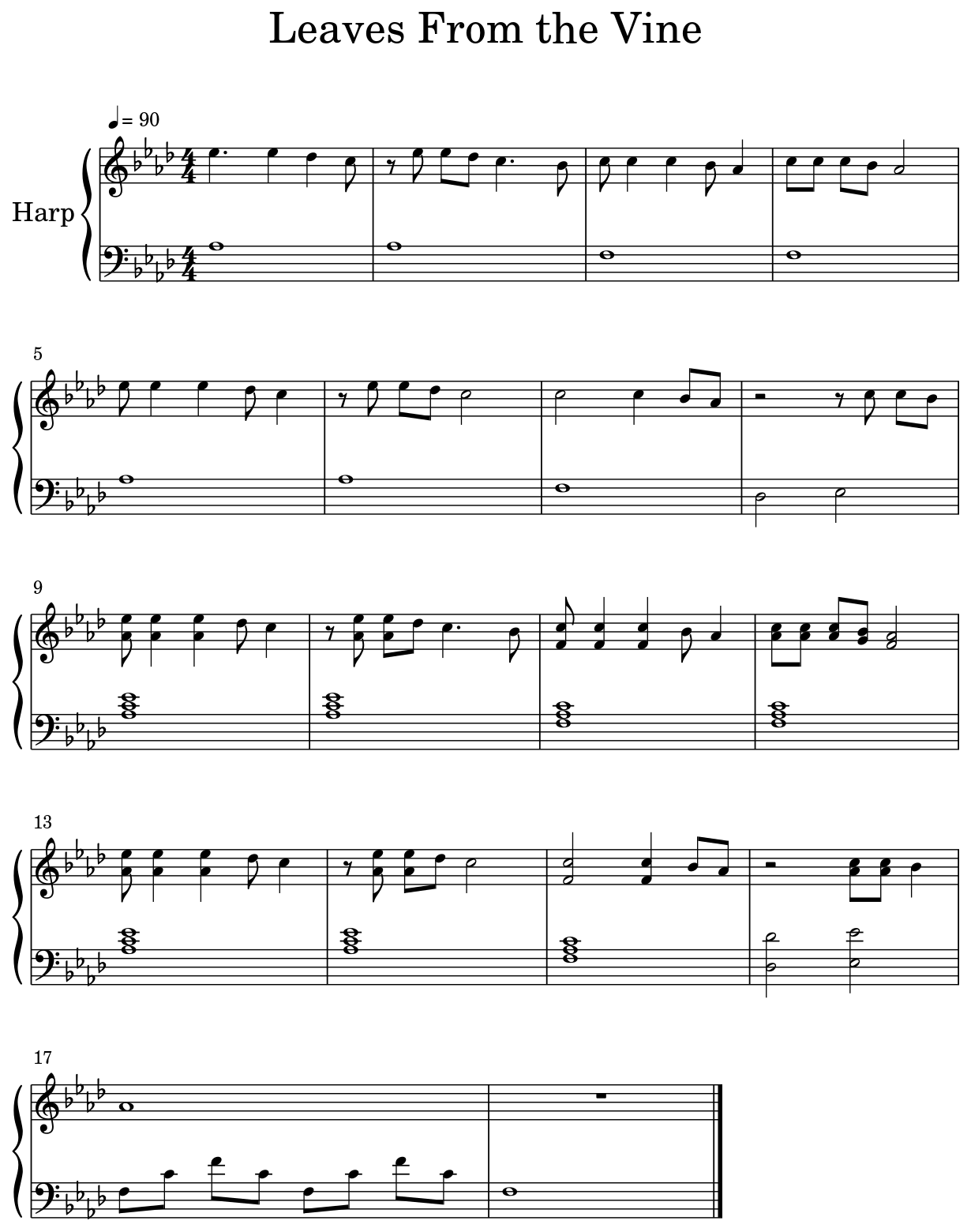
Leaves From The Vine Sheet music for Piano, Violin, Viola, Cello & more instruments (Piano Sextet) | Musescore.com

Leaves from the Vine" from 'Avatar: The Last Airbender' Sheet Music in A Major - Download & Print - SKU: MN0213426

Leaves From the Vine Sheet music for Flute, Oboe, Clarinet in b-flat, Clarinet bass & more instruments (Mixed Ensemble) | Musescore.com

Leaves From The Vine By Benjamin Wynn And Jeremy Zuckerman - Digital Sheet Music For Score And Parts - Download & Print A0.918239 | Sheet Music Plus
Leaves from the Vine" from 'Avatar: The Last Airbender' Sheet Music for Beginners in C Major - Download & Print - SKU: MN0217998

Avatar the Last Airbender- Leaves from the Vine/ Little Soldier Boy- Beginner Piano Tutorial EASY - YouTube
Avatar The Last Airbender Leaves From The Vine Sheet, HD Png Download , Transparent Png Image - PNGitem

Leaves From The Vine By Benjamin Wynn And Jeremy Zuckerman - Digital Sheet Music For Score And Parts - Download & Print A0.918239 | Sheet Music Plus