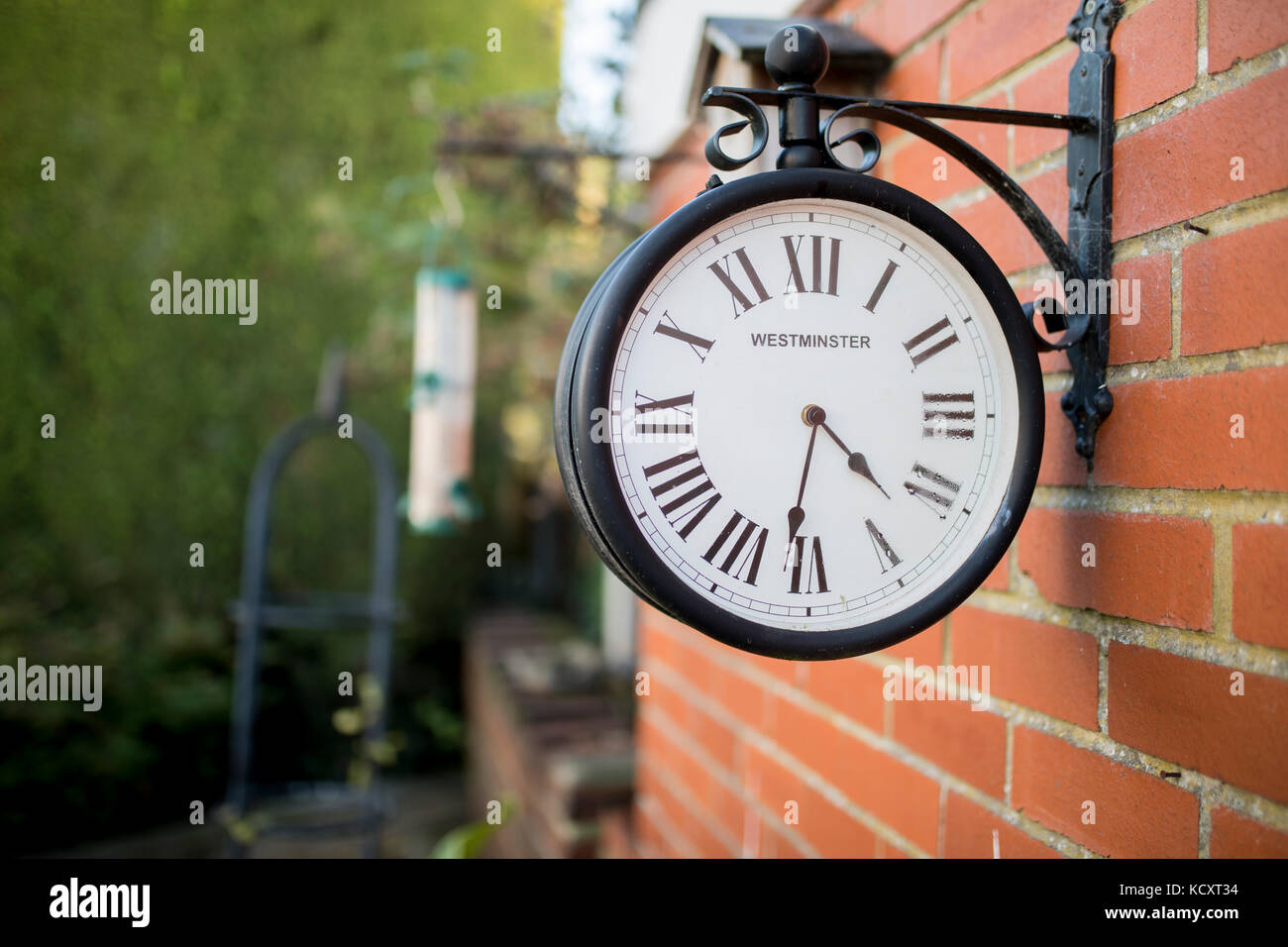
Westminster antica stazione di ricerca orologio attaccato ad un muro di mattoni in un tradizionale giardino inglese Foto stock - Alamy

Orologio da parete impermeabile con stazione ferroviaria a doppia faccia per giardino orologio da parete in metallo retrò in ferro battuto decorazione silenziosa per interni ed esterni _ - AliExpress Mobile

Relaxdays Meridiana da Giardino, Design Antico, Resistente, Autoportante, Ghisa, Orologio Solare, 31x30x21 cm, Dorato | Leroy Merlin

avvicinamento di un vecchio rotto orologio fatto di legna con un' verde pianta sospeso su un' polo nel il vivente giardino a Alba. nuovo vita e la libertà concetto 20204034 Stock Photo

kuny Grande orologio da giardino retrò, resistente alle intemperie, orologio da bagno, grande, vintage, decorativo, con senza ticchettio : Amazon.it: Casa e cucina
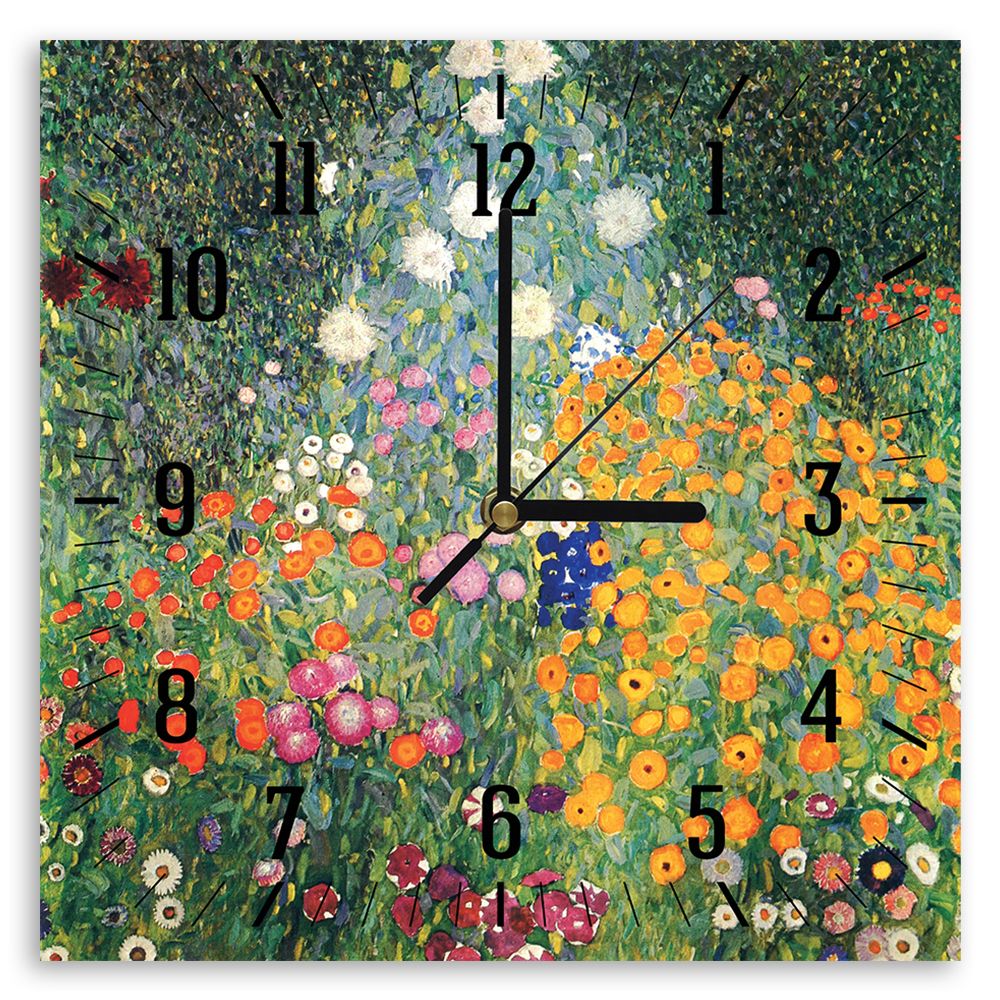
Quadri famosi, stampe su tela, posters vintage e arredo da parete - ツ Legendarte - Orologio murale - Giardino Fiorito - Gustav Klimt - Decorazione da Parete

Orologio da giardino a due lati da parete in stile vintage con copertura impermeabile Nero - Costway

OROLOGIO DA PARETE GIARDINO ROMANO GRANDE NUMERI INTERNI ESTERNI GIGANTE FACCIA APERTA METALLO 60CM | eBay

Un orologio solare può diventare una decorazione del tuo giardino. Questo è molto originale e creativo. Orologi solari | Sundial, Sundials, Garden art

Orologio da Parete da Giardino per Esterni, Orologio da Giardino retrò Grande in Ferro battuto da 23 Pollici Orologio da Esterno Impermeabile con quadrante Aperto Gigante Orologio da Esterno : Amazon.it: Giardino

Grande Orologio da Parete da Giardino Impermeabile All'aperto con Visualizzazione di Temperatura E umidità Movimento al Quarzo Silenzioso Decorazioni per Interni/Esterni Piscina Bagno Terrazza : Amazon.it: Casa e cucina















