Concepto Con Objetos Agricultura. Instrumentos Para El Cultivo De Plantas De Proceso De Plántulas, Crecimiento De Las Plantas, Fertilizantes Y Etapa De Efecto Invernadero. Ilustraciones Svg, Vectoriales, Clip Art Vectorizado Libre De

Plantas Y Elegante De Efecto Invernadero En Un Jardín Fotos, Retratos, Imágenes Y Fotografía De Archivo Libres De Derecho. Image 45630202.

Un Montón De Las Plantas De Macetas Dentro De Un Vivero De Efecto Invernadero. Fotos, Retratos, Imágenes Y Fotografía De Archivo Libres De Derecho. Image 7680164.

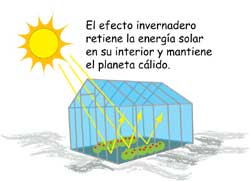
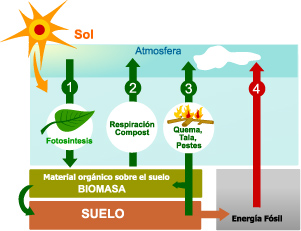
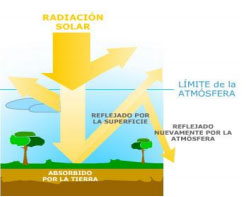
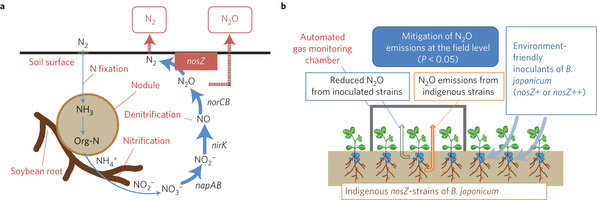
plan de compensación de compensación de carbono para reducir las emisiones de volcanes, plantas de gases

Materiales de efecto invernadero de bajo coste para las plantas de vivero de cama/banco - China Cultivar la cama, cama de riego

De Efecto Invernadero Con Las Plantas Jóvenes Fotos, Retratos, Imágenes Y Fotografía De Archivo Libres De Derecho. Image 13228042.

COMO INFLUYE LA FOTOSÍNTESIS EN EL CRECIMIENTO DE LAS PLANTAS Y EL CONSUMO DE GASES DE EFECTO - Brainly.lat

Gases de efecto invernadero tropical interior soleada llena de exuberantes plantas verdes. Jardín botánico de fondo. Cada vez más frescas hojas de plantas decorativas de interior Fotografía de stock - Alamy

Como influye la fotocintesis en el crecimiento de las plantas y el consumo de gases de efecto - Brainly.lat

LATERN Carpa de Efecto Invernadero Emergente, Mini Casa de Cultivo PVC Habitación Garden Flower Sunshine Cubierta de Invernadero Portátil para Plantas de Jardín Cold Frost Protect (70 x 70 x 80cm) :