DESARROLLO E IMPLEMENTACION DE UN SISTEMA DE CALIBRACION DE TERMOMETROS CLINICOS INFRARROJOS DE O IDO

Citizen CTA-303 Termómetro Digital Antibacterial, color Blanco : Amazon.com.mx: Salud y Cuidado Personal

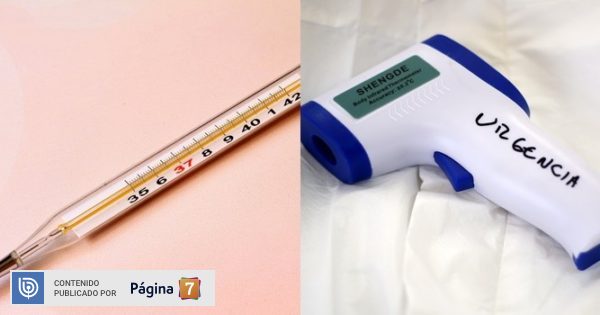
El mercurio Oral/Termómetro rectal - China Termómetro bucal Clinica Termómetro oral, rectal Termómetro Termómetro rectal


:format(jpg):quality(99):watermark(f.elconfidencial.com/file/bae/eea/fde/baeeeafde1b3229287b0c008f7602058.png,0,275,1)/f.elconfidencial.com/original/b2d/0f7/f86/b2d0f7f86b6c77f4430d500d69c9467a.jpg)














![⚡ [2022] Termómetro digital vs termómetro de mercurio: ¿cuál es mejor? [ahumados.shop] ⚡ [2022] Termómetro digital vs termómetro de mercurio: ¿cuál es mejor? [ahumados.shop]](https://www.ahumados.shop/wp-content/uploads/2021/08/mercury-thermometer-vs.-digital-thermometer.jpg)