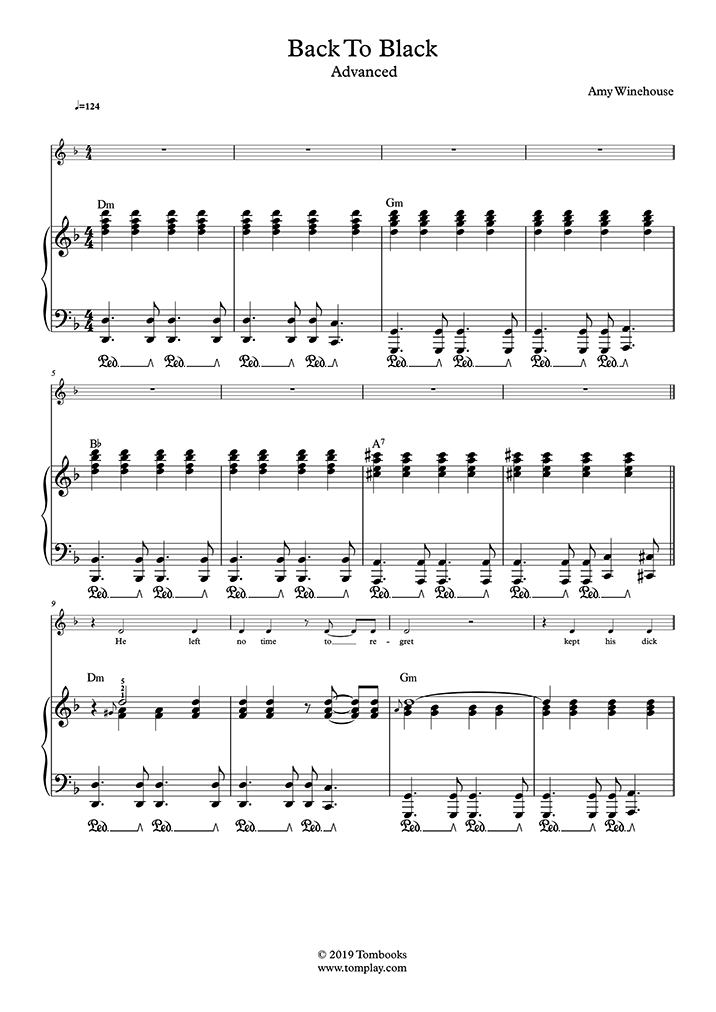
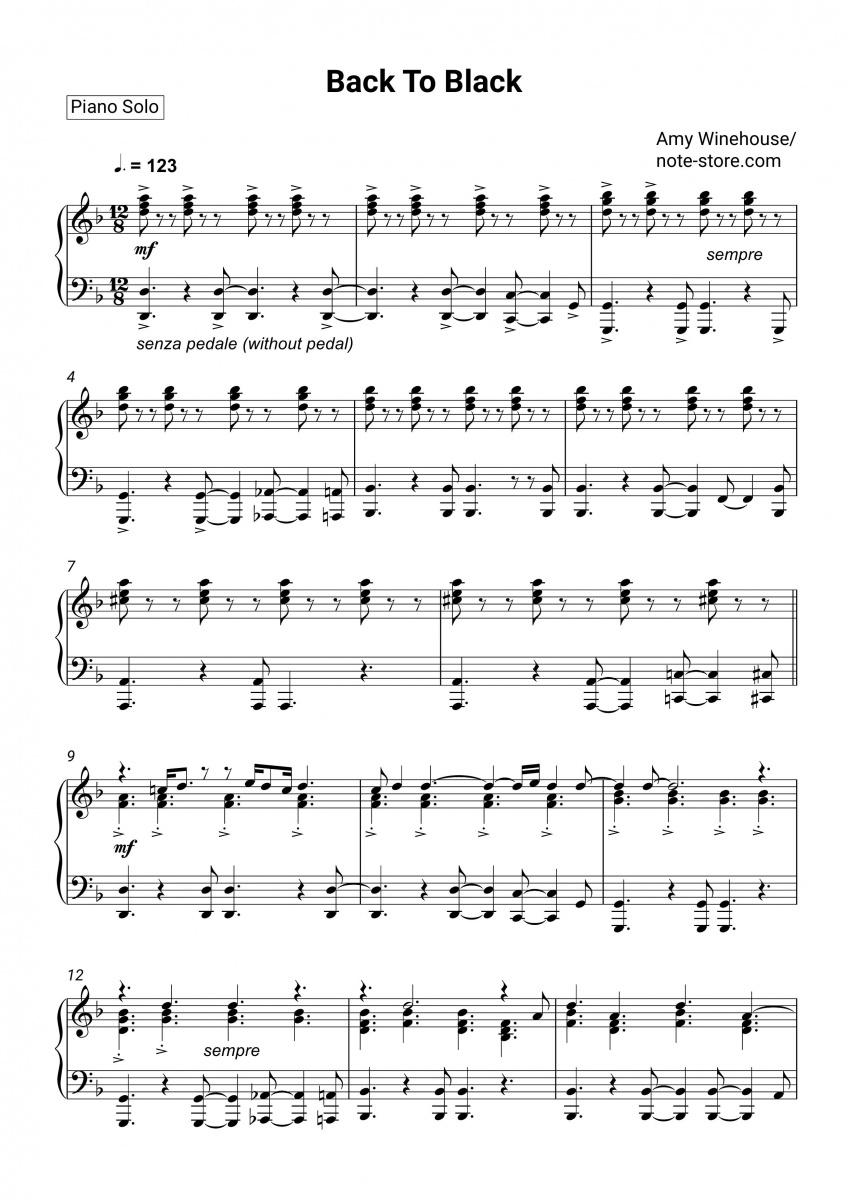
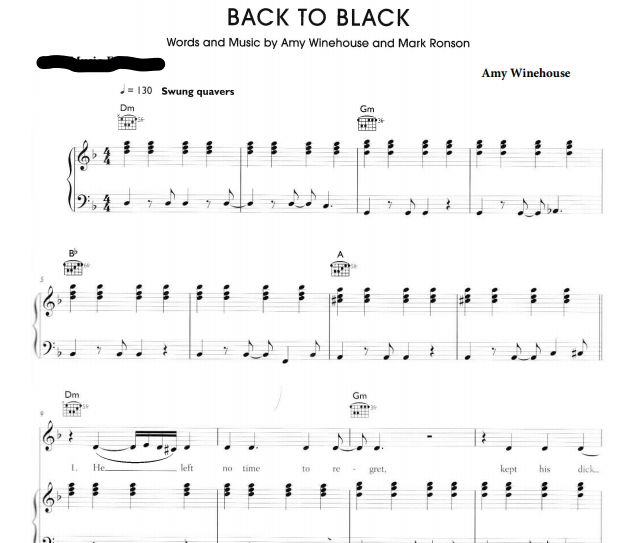
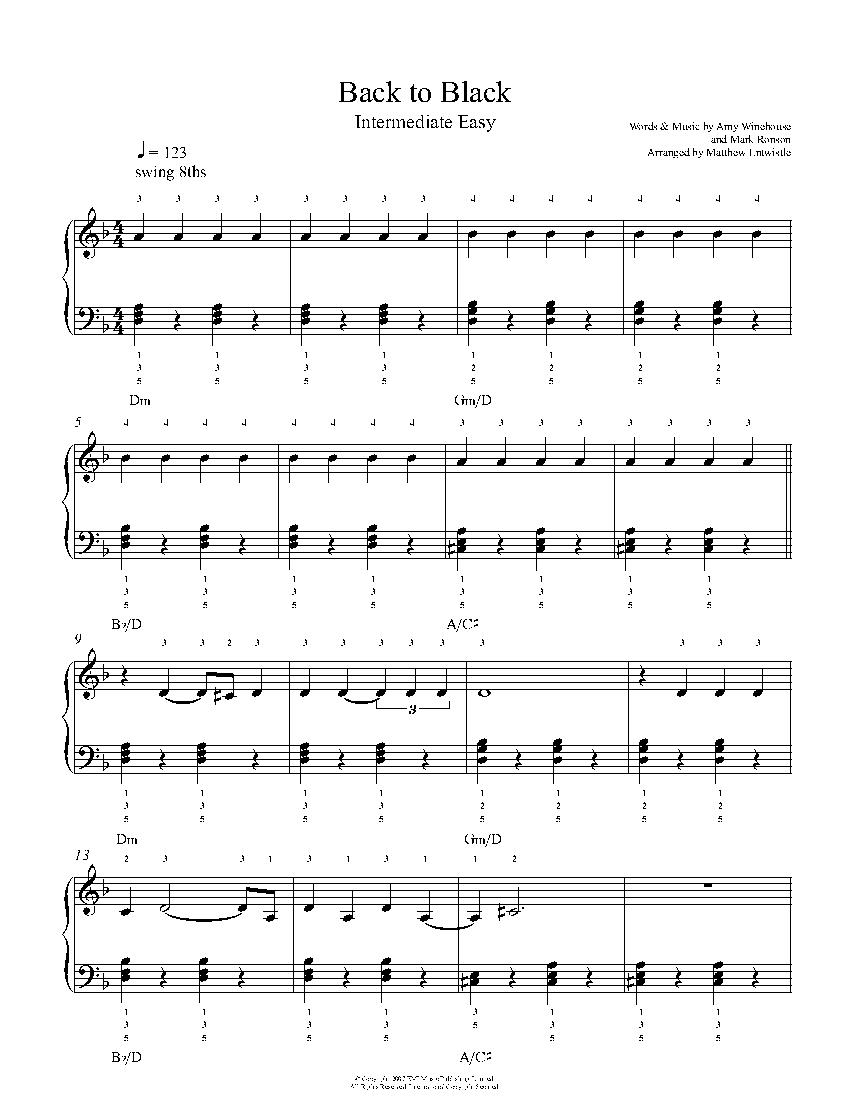
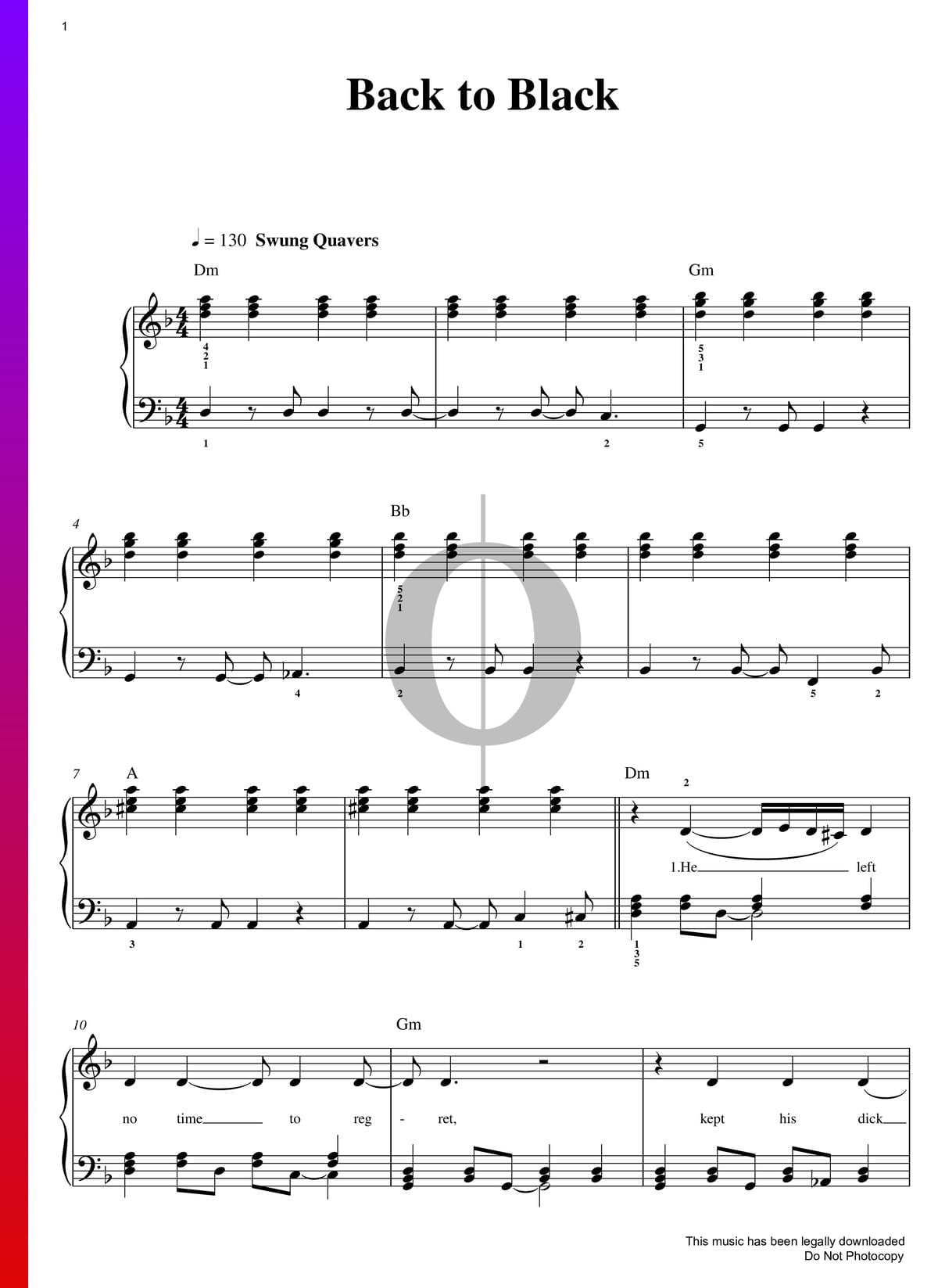
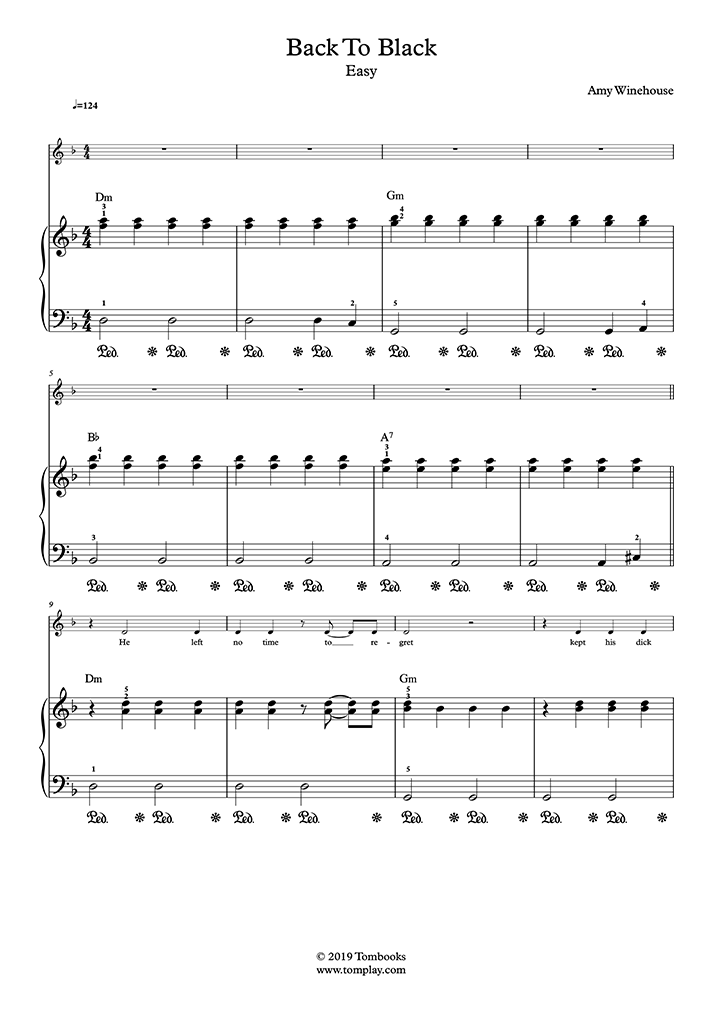
Amy Winehouse "Back to Black" Sheet Music in D Minor (transposable) - Download & Print - SKU: MN0063919

ac/dc back in black main Guitar Rif.f | Acoustic guitar music, Guitar tutorial, Guitar chords beginner

ac/dc back in black chorus guitar tab . | Guitar tabs songs, Guitar tutorials songs, Electric guitar tabs