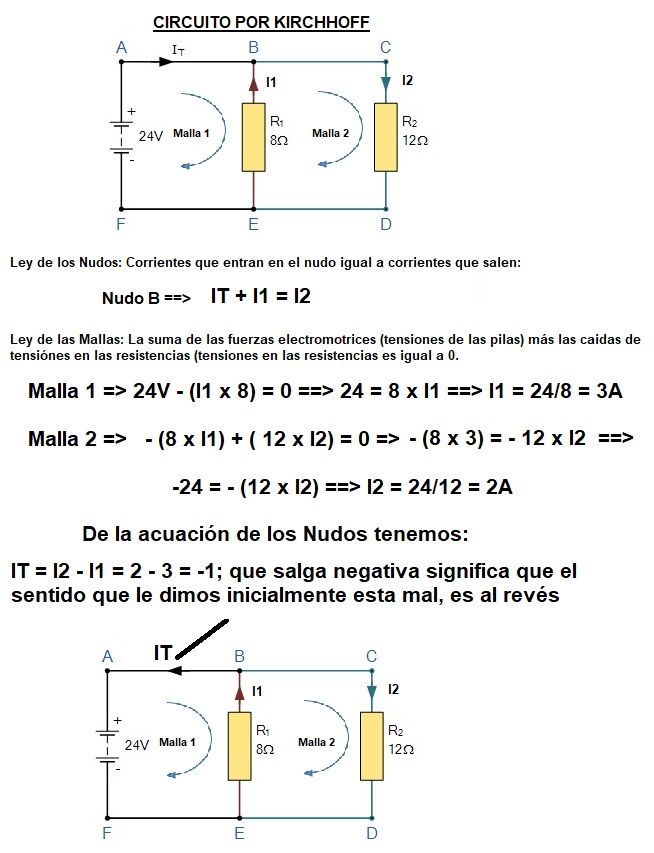
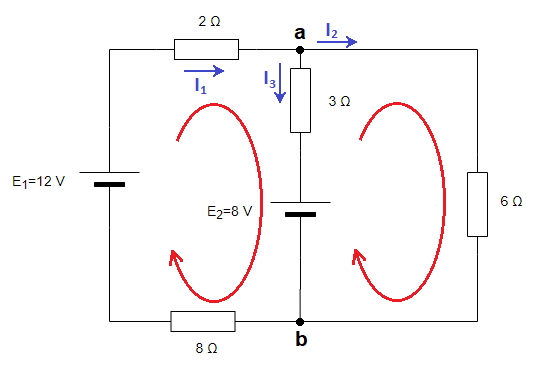
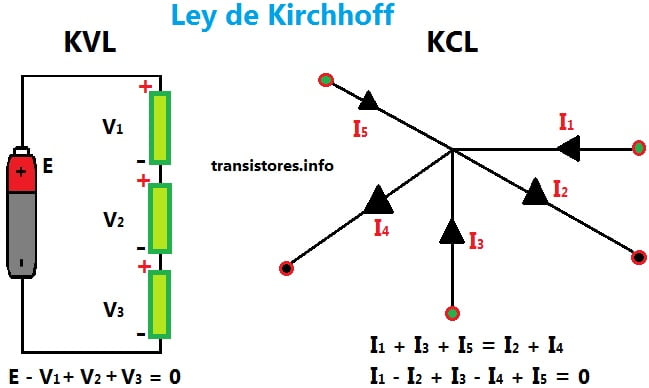
▷ Ley de Kirchhoff de Corriente: Esta ley establece que la suma de las corrientes que fluyen a través de un punto en un circuito cerrado es igual a cero. Ley de

Mónico Sánchez 2.0 ar Twitter: "#TalDiaComoHoy de 1824, nacía Gustav # Kirchhoff, #FísicoaAlemán. Sus contribución en la ciencia: campos de los #CircuitosEléctricos, la teoría de placas, la óptica, la espectroscopia y la emisión