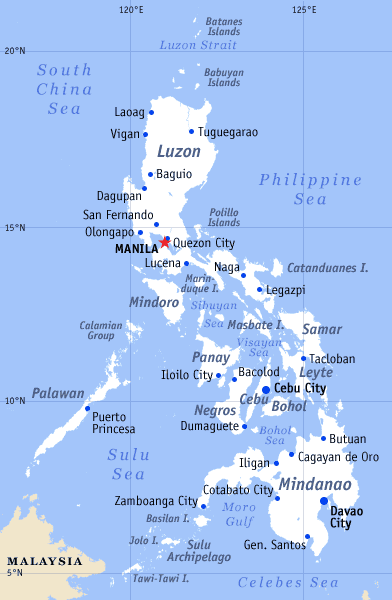
Il Paesaggio Urbano Di Manila, Con I Bassifondi Ed I Grattacieli Porto Marittimo E Zone Residenziali Il Contrasto Di Povero E Dei Immagine Stock - Immagine di porto, asia: 152247671

La Città Di Manila, Capitale Delle Filippine Immagine Stock - Immagine di bacino, distretto: 160749243

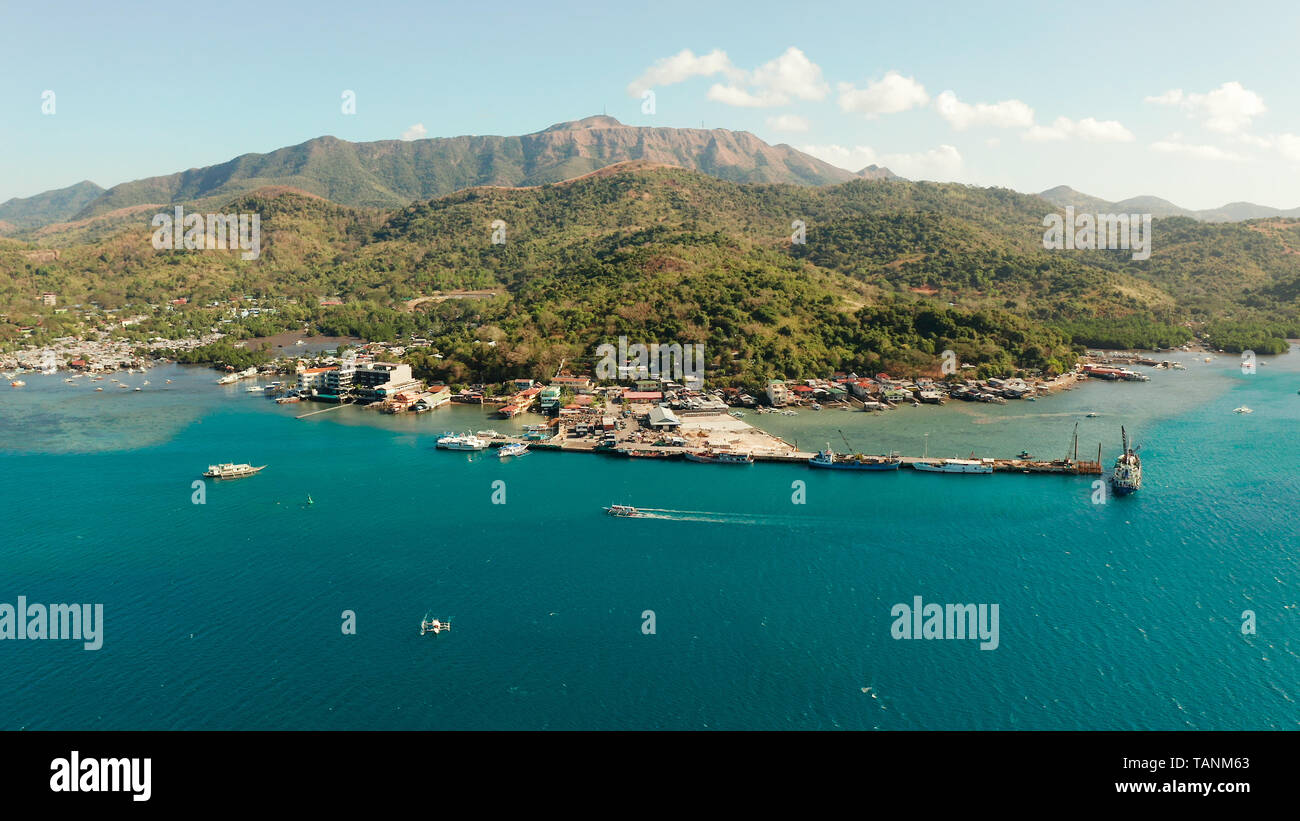
Immagini Stock - Villaggio Di Palafitte Costruito Sul Mare, Vista Dall'alto. Città E Porto Sull'isola Di Balabac, Palawan, Filippine.. Image 129601058.

Città Di Manila La Capitale Delle Filippine Con Edifici Moderni. Vista Aerea. Fotografia Editoriale - Immagine di lifestyles, asiatico: 222525136

Città E Porto Delle Filippine Di Palawan Isola Di Balabac. Fotografia Stock - Immagine di barca, casa: 204930000