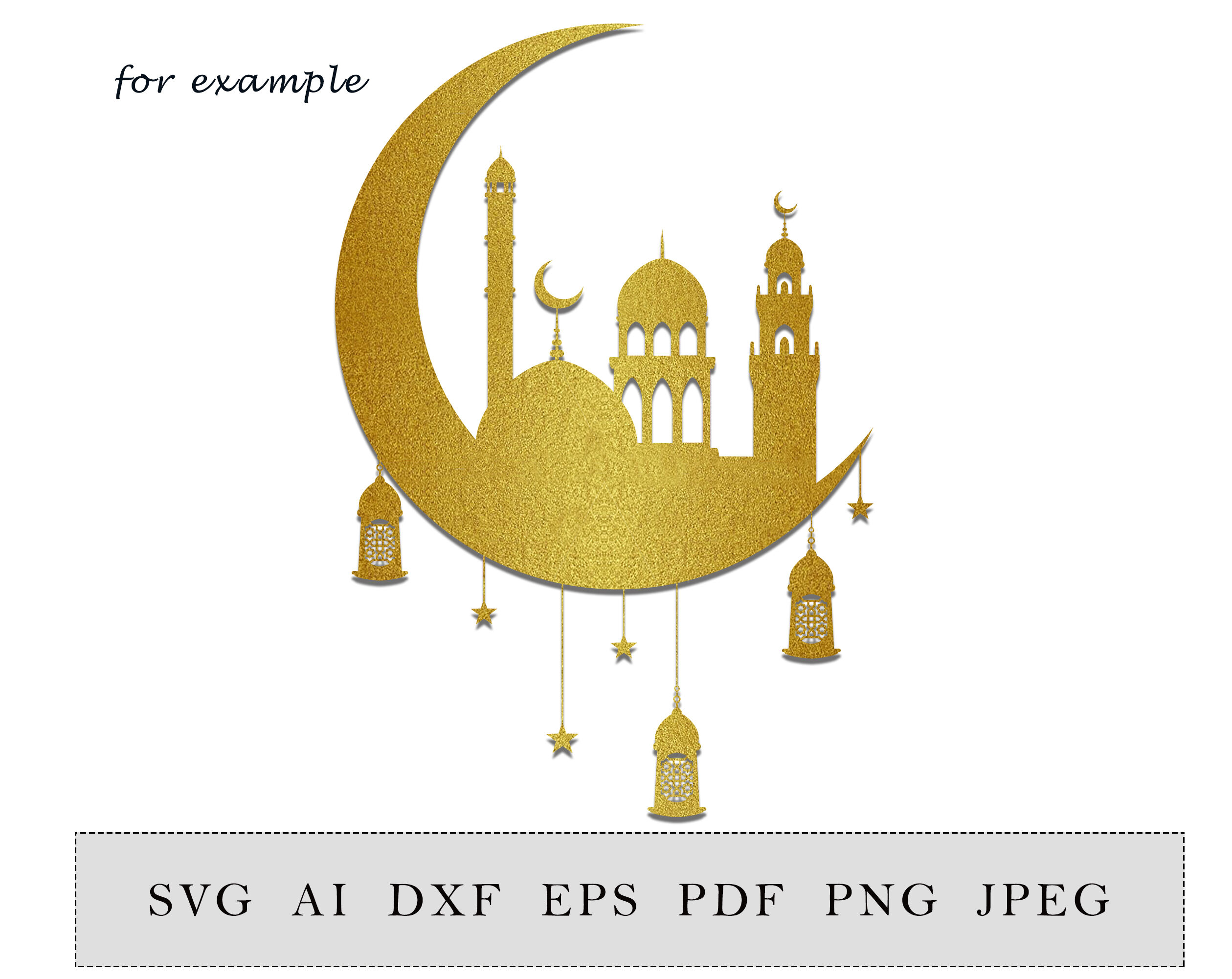
Crescent with lantern and mosque, ramadan decoration, islamic home decor, digital. Cut file, SVG, DXF, PNG file. By ESHA | TheHungryJPEG

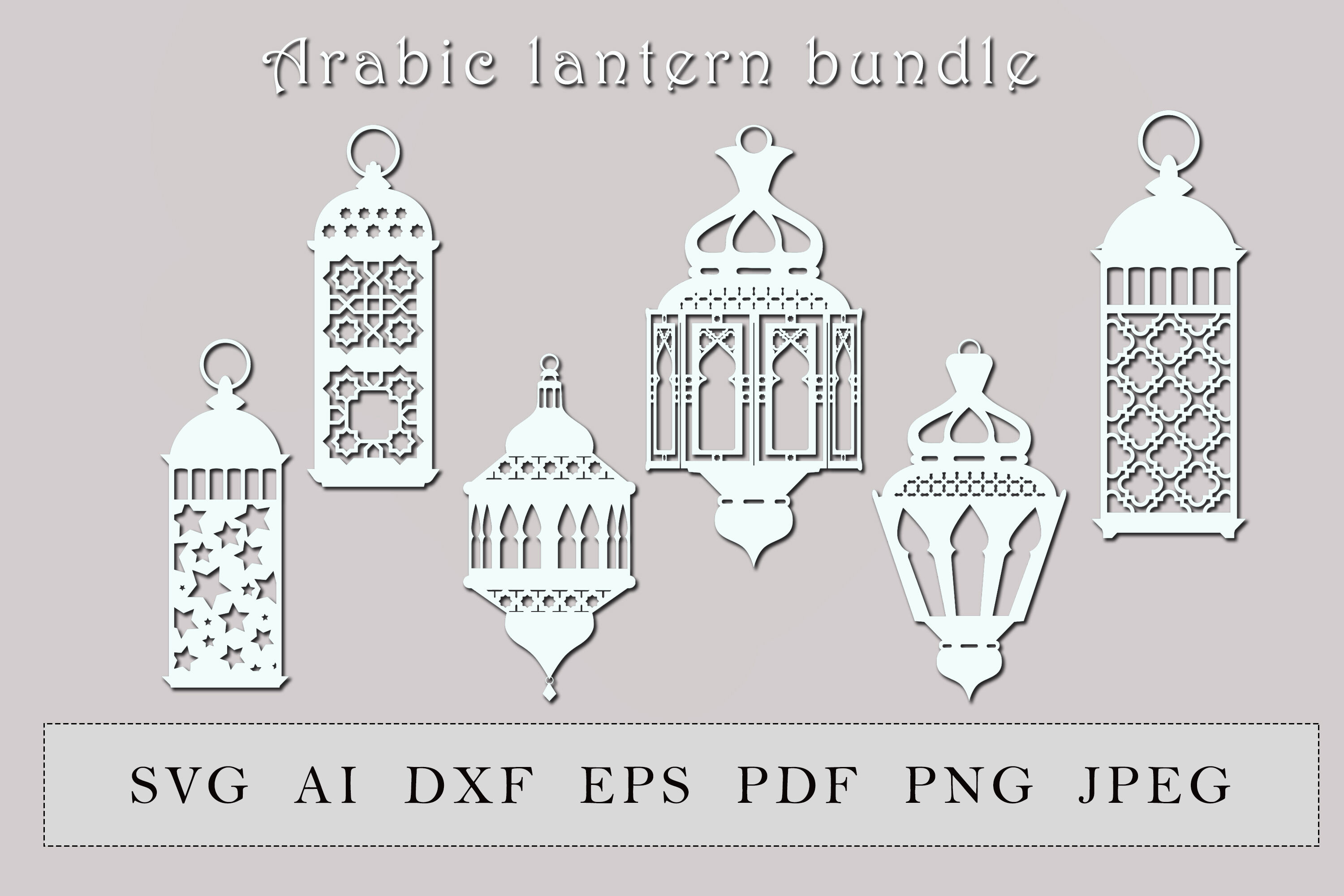
Turkish Lanterns svg, Ramadan svg, celebration svg, Turkish décor svg, cut files for Cricut, Silhouette Design, Svg, PNG, Dxf - The Silhouette Queen