Lápis de Cor Tradicional Superior Faber-Castell | Lister - Lápis de Cor Verde Cromo Opaco 174 - Polychromos Faber-Castell - Redondo - 1un - Faber-Castell

Lápis de Cor Tradicional Superior Faber-Castell | Lister - Lápis de Cor Verde Folha 112 - Polychromos Faber-Castell - Redondo - 1un - Faber-Castell

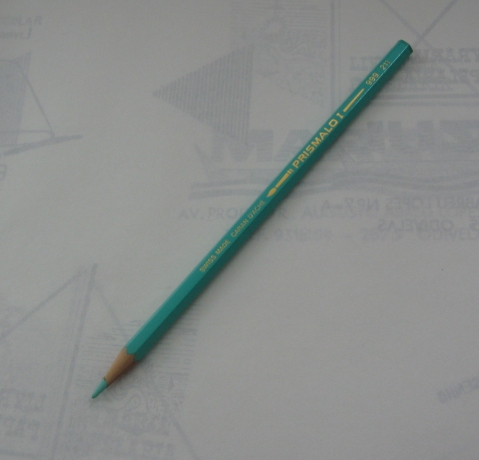
Como eu amo desenhar então nada mais justo que colocar um degradê básico de verde. Pra nós que gostam… | Green inspiration, Green aesthetic, Green gemstones jewelry