Falco - Beatles Medley: Baby You Can Drive My Car / She Loves You / Back in the Ussr MP3 Download & Lyrics | Boomplay
London Session Singers - Back In The USSR ft. J Lennon & P McCartney MP3 Download & Lyrics | Boomplay
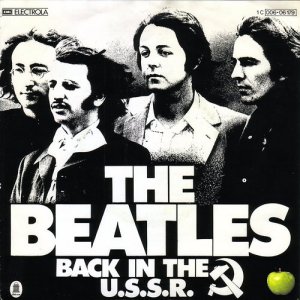
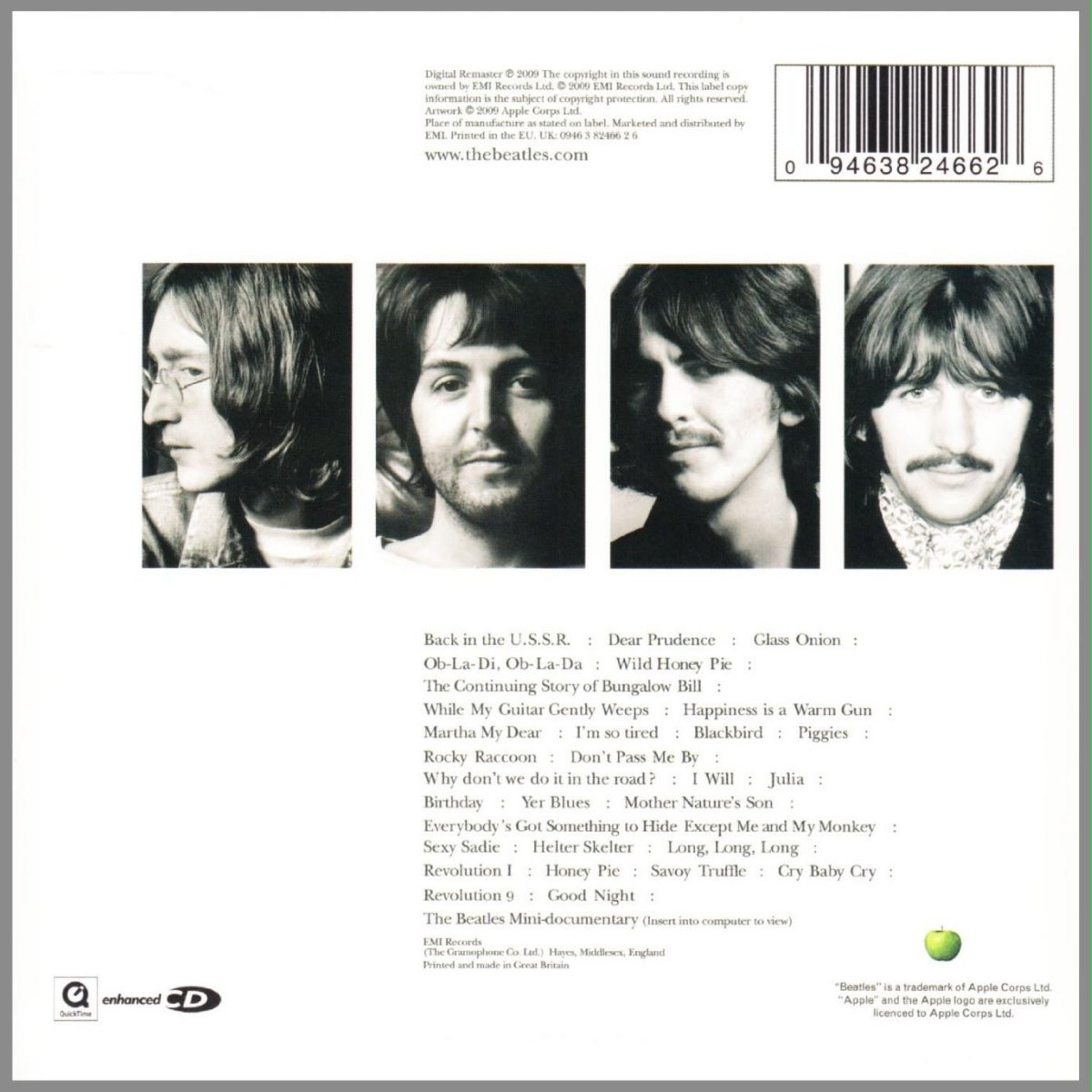
Back in the U.S.S.R. / Don't Pass Me By by The Beatles (Single, Pop Rock): Reviews, Ratings, Credits, Song list - Rate Your Music
![Back In The U.S.S.R. [Jazz version] sheet music (real book with lyrics) Back In The U.S.S.R. [Jazz version] sheet music (real book with lyrics)](https://cdn3.virtualsheetmusic.com/images/first_pages/HL/HL-453856First_BIG.png)




:strip_exif():format(jpg)/http://s3-ap-south-1.amazonaws.com/wynk-music-cms/srch_wmg/music/update/018777380164/1656299508/srch_wmg_A10302B00002923592.jpg)

:strip_exif():format(jpg)/http://s3.ap-south-1.amazonaws.com/wynk-music-cms/srch_wmg/20230330023634760/4050538668599/1680146727988/resources/4050538668599.jpg)