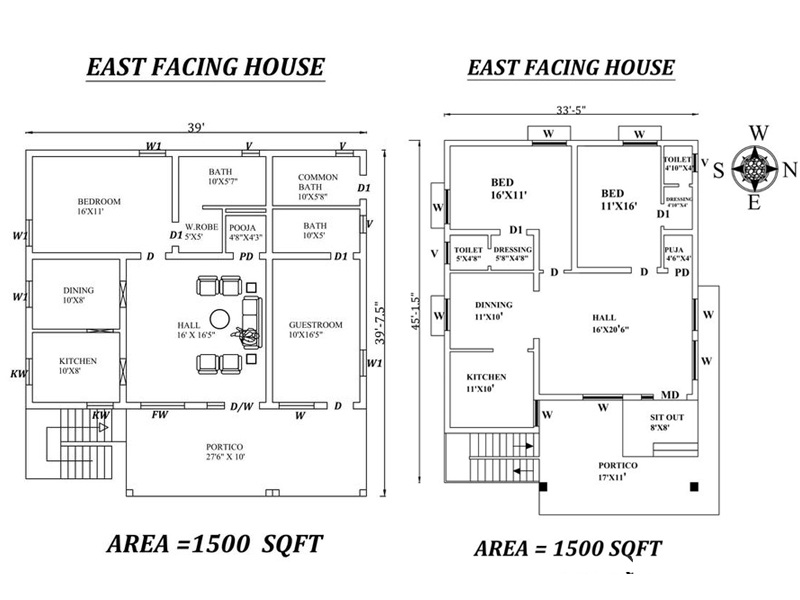
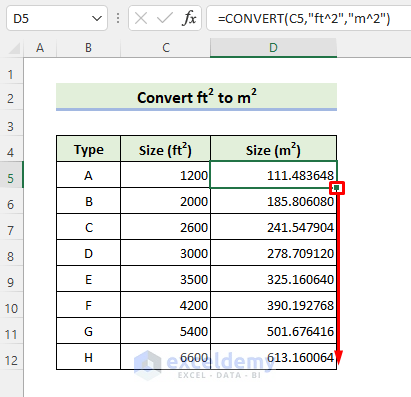
30x40 West Facing House Plans | 1200 Square Feet House Design | West Facing 3BHK House Plans - YouTube

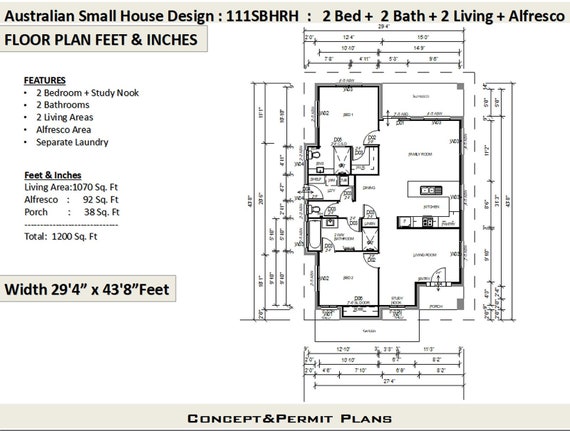
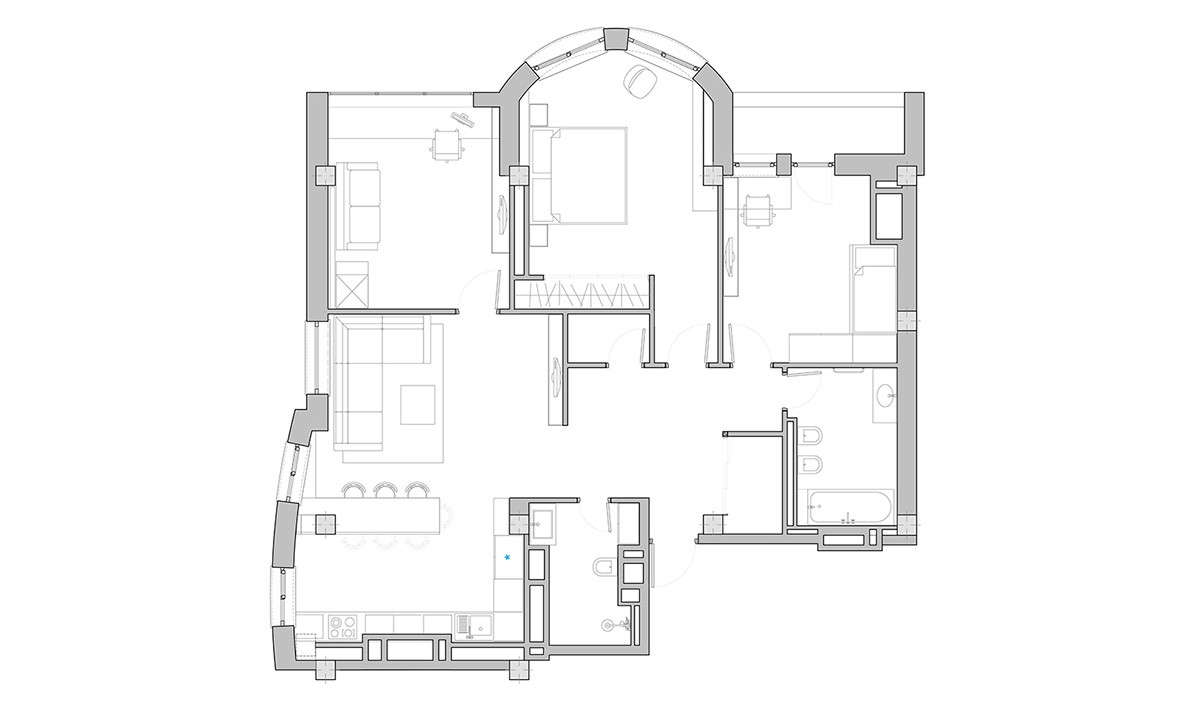
1200 sq-ft Rs.18 lakhs cost estimated house plan - Kerala home design and floor plans - 9K+ house designs

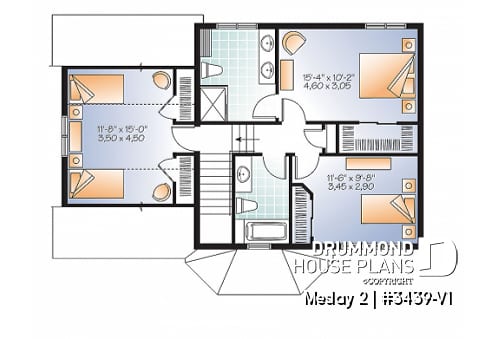
Image result for duplex house plans india 1200 sq ft | House design photos, Bungalow house design, House front design

30X40 Feet, 1200 Sqft House Design with 2 Entrance, Shaded Terrace Louvered | 9X12 Meter | ID-081 - YouTube