Persian Design Red Carpet of Flowers for Family Room/Majlis in Modern Home/Private Villa - China Living Room Carpet Decorating Ideas and Living Room Carpet Colours price

Amazon.com: Unique Loom Solid Shag Collection Area Rug (3' 3" x 5' 3" Rectangle, Cherry Red) : Home & Kitchen

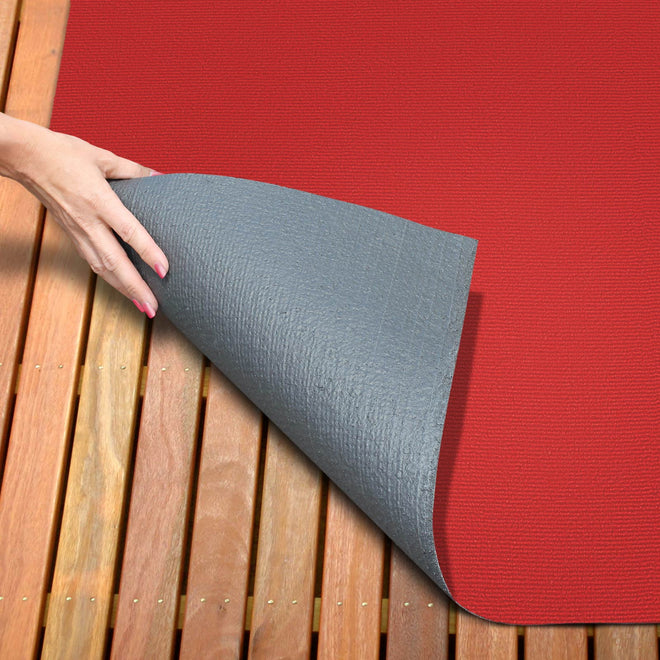
Amazon.com: Sweet Home Stores SH Collection Solid Rubberback Indoor Runner Rug, 20" x 59", Red : Home & Kitchen

Deluxe Ceremonial Red Carpet | Ceremonial Groundbreaking, Grand Opening , Crowd Control & Memorial Supplies