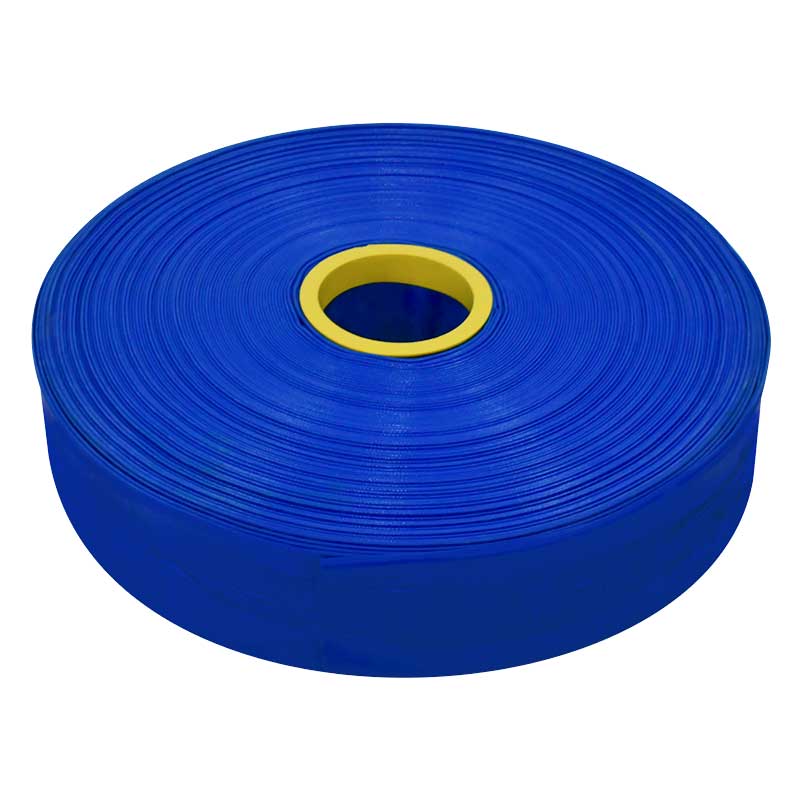
Amazon.com: Mangueras de jardín de 16.4 ft a 147.6 ft, manguera de agua extensible, para riego agrícola, herramienta de riego agrícola, manguera de agua ligera con duradera (color rosa, longitud: 98.4 ft) :

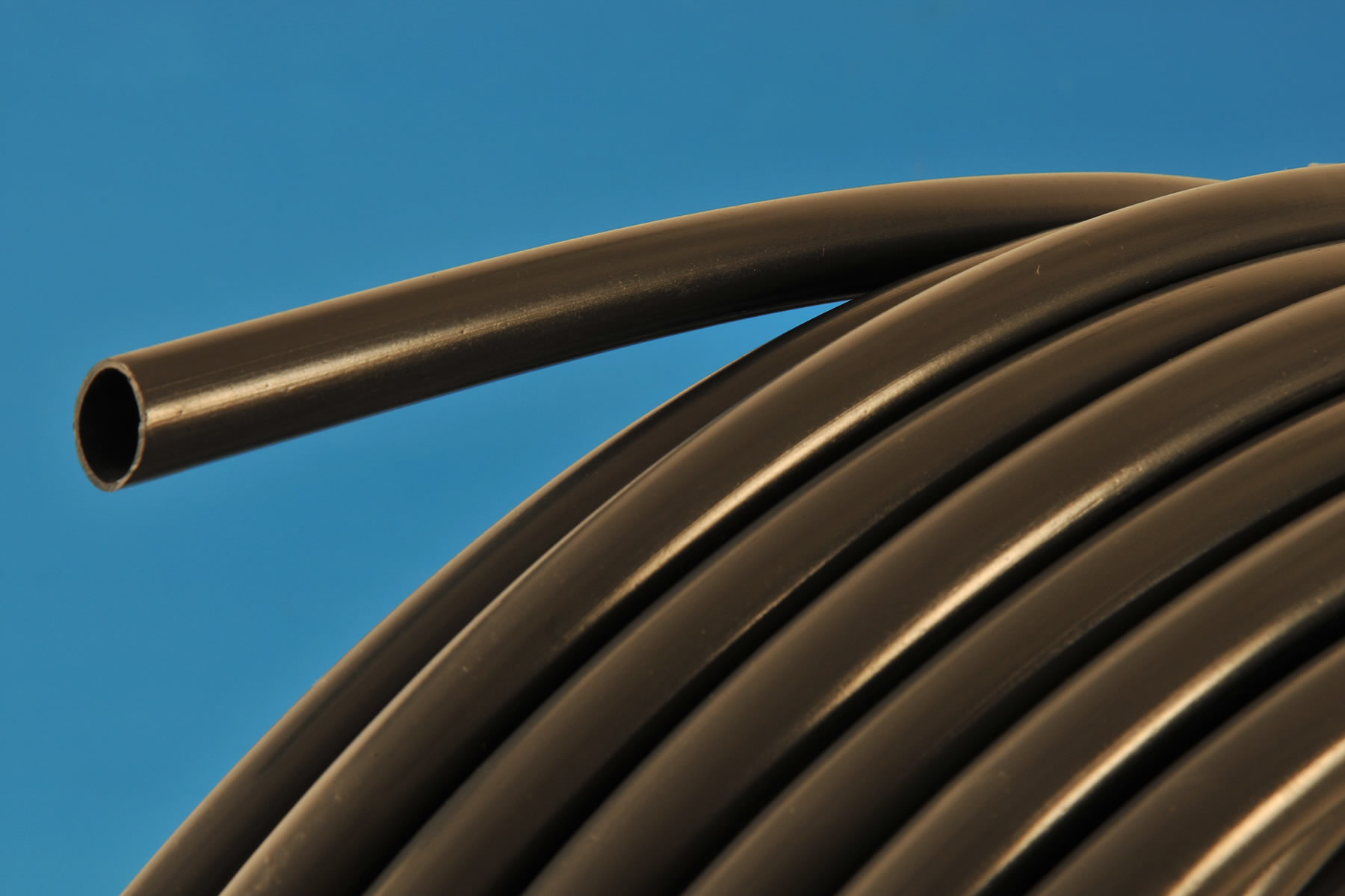
Manguera de Polietileno 3/4″ para Riego Agrícola Instalación Superficial o Enterrada Rollo de 100 Metros – Bedon