SCULPFUN S10 Incisione Laser, 10W modulo laser Incisore con cavo Air Assist, precisione di taglio 0,01 mm, qualità industriale, Bereich410*420mm : Amazon.it: Fai da te

Refrigeratore per acqua industriale per macchina per incisione laser Co2, incisione laser : Amazon.it: Casa e cucina

OMTech 100W Incisore Laser CO2, Taglierina Laser 600x1000MM, Macchina da Taglio Industriale per Incisione Laser con Controller Ruida Autofocus Autolift Ruote Assistite ad Aria a 2 Vie : Amazon.it: Fai da te
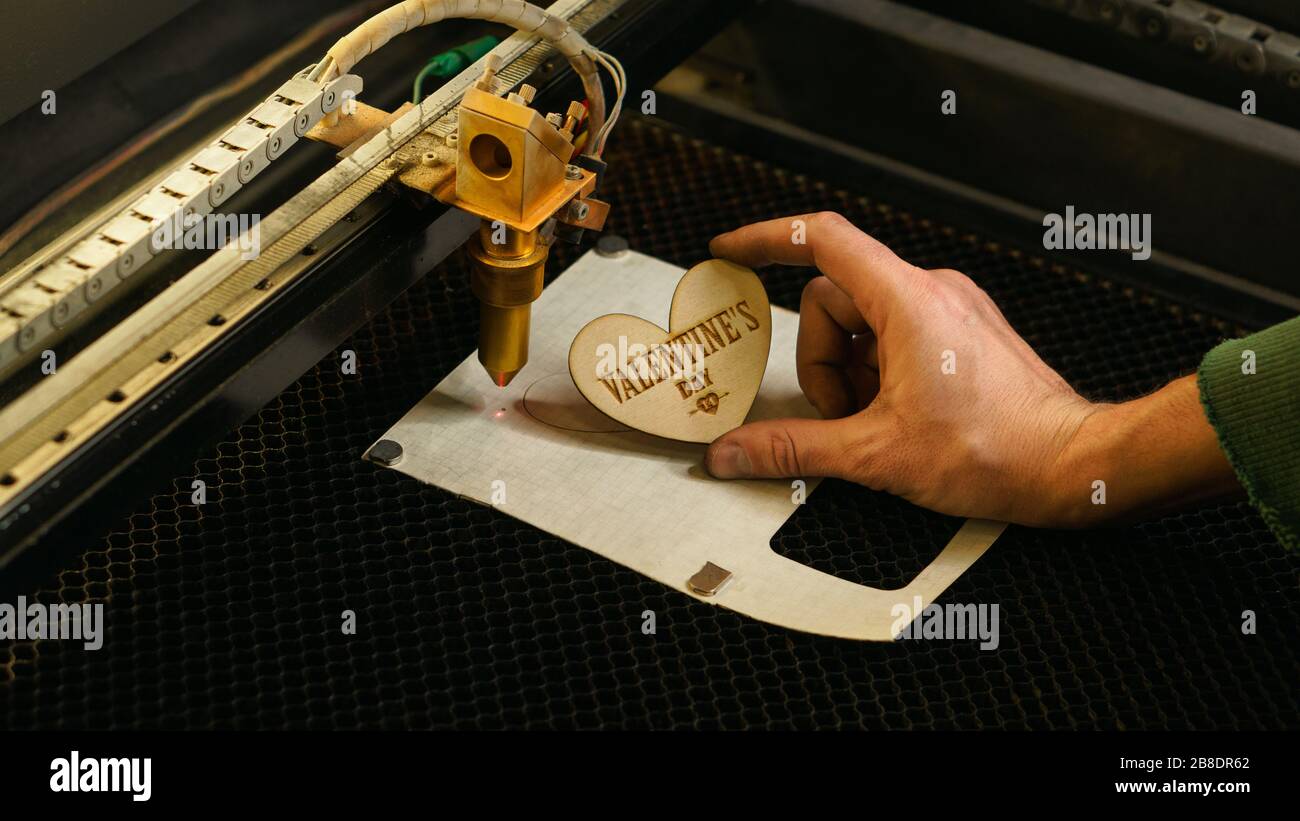
Raggio di taglio laser ad alta precisione su un foglio di compensato. Tecnologia moderna di taglio del legno. Taglio laser legno 3d simbolo del giorno di San Valentino. Incisione laser industriale. Laser

Raggio di taglio laser ad alta precisione su un foglio di compensato. Tecnologia moderna di taglio del legno. Taglio laser legno 3d simbolo del giorno di San Valentino. Incisione laser industriale. Laser CNC. Masterclass, officina Foto stock - Alamy

Macchine taglio incisione e marcatura LASER | Pantografi e macchine taglio e incisione laser - Progettazione produzione e vendita

OMTech 100W Incisore Laser CO2, Taglierina Laser 600x1000MM, Macchina da Taglio Industriale per Incisione Laser con Controller Ruida Autofocus Autolift Ruote Assistite ad Aria a 2 Vie : Amazon.it: Fai da te